Restless Legs Syndrome (RLS)
Author: Giselle Robel
Giselle Robel
Category: Health
Restless leg syndrome, or RLS, is a neurological disorder, also known as Willis-Ekbom disease or RLS/WED.
Restless legs syndrome (RLS) is a condition that causes an uncontrollable urge to move your legs, usually because of an uncomfortable sensation. It typically happens in the evening or nighttime hours when you’re sitting or lying down. Moving eases the unpleasant feeling temporarily.
Restless legs syndrome can begin at any age and generally worsens as you age. It can disrupt sleep.
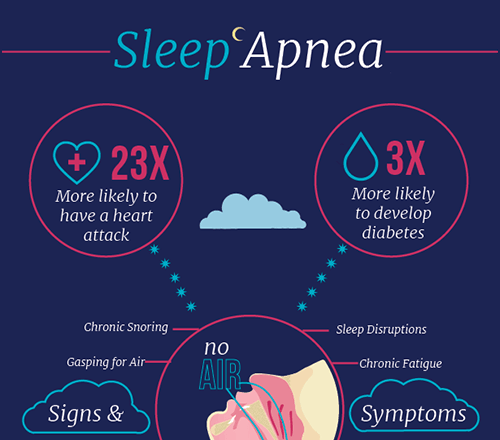
The most serious concern for people with RLS is that since it disrupts sleep, causes daytime sleepiness and fatigue. RLS and sleep deprivation can put you at risk for other health problems, including depression if not treated.
Symptoms of Restless Leg Syndrome
The chief symptom is an urge to move the legs. Common accompanying characteristics of RLS include:
- Sensations that begin after rest. The sensation typically begins after you’ve been lying down or sitting for an extended time, such as in a car, airplane or movie theater.
- Relief with movement. The sensation of RLS lessens with movement, such as stretching, jiggling your legs, pacing or walking.
- Worsening of symptoms in the evening. Symptoms occur mainly at night.
- Nighttime leg twitching. RLS may be associated with another, more common condition called periodic limb movement of sleep, which causes your legs to twitch and kick, possibly throughout the night, while you sleep.
People typically describe RLS symptoms as abnormal, unpleasant sensations in their legs or feet. They usually happen on both sides of the body. Less commonly, the sensations affect the arms.
The sensations, which generally occur within the limb rather than on the skin, are described as:
- Crawling
- Creeping
- Pulling
- Throbbing
- Aching
- Itching
- Electric
Sometimes the sensations are difficult to explain. People with RLS usually don’t describe the condition as a muscle cramp or numbness. They do, however, consistently describe the desire to move their legs.
It’s common for symptoms to fluctuate in severity. Sometimes, symptoms disappear for periods of time, then come back.
What causes restless leg syndrome?
More often than not, the cause of RLS is a mystery. There may be a genetic predisposition and an environmental trigger.
More than 40 percent of people with RLS have some family history of the condition. In fact, there are five gene variants associated with RLS. When it runs in the family, symptoms usually start before age 40.
There may be a connection between RLS and low levels of iron in the brain, even when blood tests show that your iron level is normal.
RLS may be linked to a disruption in the dopamine pathways in the brain. Parkinson's disease is also related to dopamine. That may explain why many people with Parkinson's also have RLS. Some of the same medications are used to treat both conditions. Research on these and other theories is ongoing.
It's possible that certain substances like caffeine or alcohol can trigger or intensify symptoms. Other potential causes include medications to treat:
- allergies
- nausea
- depression
- psychosis
Primary RLS isn't related to an underlying condition. But RLS can actually be an offshoot of another health problem, like neuropathy, diabetes, or kidney failure. When that's the case, treating the main condition may resolve RLS issues.
Diagnosing restless leg syndrome
There isn't one single test that can confirm or rule out RLS. A large part of the diagnosis will be based on your description of symptoms.
To reach a diagnosis of RLS, all the following must be present:
- overwhelming urge to move, usually accompanied by strange sensations
- symptoms get worse at night and are mild or absent in the early part of the day
- sensory symptoms are triggered when you try to relax or sleep
- sensory symptoms ease up when you move
Even if all the criteria are met, you'll probably still need a physical examination. Your doctor will want to check for other neurological reasons for your symptoms.
Be sure to provide information about any over-the-counter and prescription medications and supplements you take. And tell your doctor if you have any known chronic health conditions.
Blood tests will check for iron and other deficiencies or abnormalities. If there's any sign that something besides RLS is involved, you may be referred to a sleep specialist, neurologist, or other specialists.
It may be harder to diagnose RLS in children who aren't able to describe their symptoms.
Medications for restless leg syndrome
Medication won't cure RLS, but it can help manage symptoms. Some options are:
Drugs that increase dopamine (dopaminergic agents)
These medications help decrease motion in your legs.
Drugs in this group include:
- pramipexole (Mirapex)
- ropinirole (Requip)
- rotigotine (Neupro)
Side effects may include mild lightheadedness and nausea. These medications can become less effective over time. In some people, they can cause daytime sleepiness impulse control disorders, and worsening of RLS symptoms.
Sleep aids and muscle relaxants (benzodiazepines)
These medications don't completely eliminate symptoms, but they can help you relax and sleep better.
Drugs in this group include:
- clonazepam (Klonopin)
- eszopiclone (Lunesta)
- temazepam (Restoril)
- zaleplon (Sonata)
- zolpidem (Ambien)
Side effects include daytime sleepiness.
Narcotics (opioids)
These medications can decrease pain and strange sensations and help you relax.
Drugs in this group include:
- codeine
- oxycodone (Oxycontin)
- combined hydrocodone and acetaminophen (Norco)
- combined oxycodone and acetaminophen (Percocet, Roxicet)
Side effects may include dizziness and nausea. You should not use these products if you have sleep apnea. These medicines are powerful and addicting.
Anticonvulsants
These medications help lessen sensory disturbances:
- gabapentin (Neurontin)
- gabapentin enacarbil (Horizant)
- pregabalin (Lyrica)
Side effects may include dizziness and fatigue.
It may take several attempts before you find the right medication. Your doctor will adjust the medication and dosage as your symptoms change.
Home remedies for restless leg syndrome
Home remedies, while unlikely to completely eliminate symptoms, may help reduce them. It may take some trial and error to find the remedies that are most helpful.
Here are a few you can try:
- Reduce or eliminate your intake of caffeine, alcohol, and tobacco.
- Strive for a regular sleep schedule, with the same bedtime and wake-up time every day of the week.
- Get some exercise every day, such as walking or swimming.
- Massage or stretch your leg muscles in the evening.
- Soak in a hot bath before bed.
- Use a heating pad or ice pack when you experience symptoms.
- Practice yoga or meditation.
When scheduling things that require prolonged sitting, such as a car or plane trip, try to arrange them for earlier in the day rather than later.
If you have an iron or other nutritional deficiency, ask your doctor or nutritionist how to improve your diet. Talk to your doctor before adding dietary supplements. It can be harmful to take certain supplements if you aren't deficient.
These options may be useful even if you take medication to manage RLS.
Risk factors for restless leg syndrome
There are certain things that may put you in a higher risk category for RLS. But it's uncertain if any of these factors actually cause RLS.
Some of them are:
- Gender : Women are twice as likely as men to get RLS.
- Age : Although you can get RLS at any age, it's more common and tends to be more severe after middle age.
- Family history : you're more likely to have RLS if others in your family have it.
- Pregnancy : Some women develop RLS during pregnancy, particularly in the last trimester. This usually resolves within weeks of delivery.
- Chronic diseases : Conditions such as peripheral neuropathy, diabetes, and kidney failure, may lead to RLS. Often treating the condition relieves symptoms of RLS.
- Medications : Antinausea, antipsychotic, antidepressant, and antihistamine medications may trigger or aggravate symptoms of RLS.
- Ethnicity : Anyone can get RLS, but it's more common in people of Northern European descent.
Having RLS can affect your overall health and quality of life. If you have RLS and chronic sleep deprivation, you may be at a higher risk of:
- heart disease
- stroke
- diabetes
- kidney disease
- depression
- early death