Narcolepsy: What It’s Like To Be
Author: Alvin
Alvin
Category: Mental Health

How is narcolepsy defined?
Narcolepsy is a long-term neurological condition that impairs the brain’s capacity to regulate sleep-wake cycles. Individuals with narcolepsy may feel relaxed at awakening but subsequently, feel extremely sleepy for most of the day. Numerous patients with narcolepsy also experienced irregular and interrupted sleep, including repeated awakenings during the night.
Narcolepsy has a significant impact on daily activities. Individuals may fall asleep unintentionally while engaged in an activity such as driving, eating, or conversing. Other symptoms may include rapid muscle weakness that causes a person to collapse or become immobile (cataplexy), vivid dream-like pictures or hallucinations, and total paralysis right before falling asleep or shortly after waking up (sleep paralysis).
After around 60 to 90 minutes in a normal sleep cycle, a person enters rapid eye movement (REM) sleep. Dreams occur during REM sleep, and the brain prohibits people from acting out their dreams during this stage of sleep. Narcoleptics usually enter rapid eye movement (REM) sleep within 15 minutes after falling asleep. Additionally, REM sleep’s muscle weakness and dream activity might occur during alertness or be missing throughout sleep. This helps to explain certain narcolepsy symptoms.
Narcolepsy, if left undiagnosed or untreated, can impair psychological, social, and cognitive function and development, as well as academic, work, and social activities.
Who is afflicted with narcolepsy?
Males and females are equally affected by narcolepsy. Although symptoms typically begin in infancy, adolescence, or young adulthood (ages 7 to 25), they can occur at any age. Narcolepsy is estimated to affect between 135,000 and 200,000 people in the United States. However, because this ailment is frequently misdiagnose, the figure may be greater. Due to the frequent misdiagnosis of patients with narcolepsy with other ailments, such as psychiatric disorders or emotional problems, might take years for someone to receive the correct diagnosis.
What are the signs and symptoms?
While narcolepsy is a chronic condition, it often does not deteriorate with age. While symptoms may lessen in part over time, they will never totally disappear. Excessive daytime sleepiness, cataplexy, sleep paralysis, and hallucinations are the most common symptoms. While everyone experiences excessive daytime sleepiness, only about 10% to 25% of affected individuals will experience all other symptoms during their illness.
Paralysis during sleep. . Sleep paralysis is similar to cataplexy but occurs on the eve of sleep. As is the case with cataplexy, individuals retain complete consciousness. Even when severe cataplexy and sleep paralysis do not result in lasting dysfunctionindividuals rapidly regain their full capacity for movement and speech following episodes.
Hallucinations. Sleep paralysis can extremely vivid and frightening pictures that typically occur as people are going asleep or waking up. Although the material is frequently predominantly visual, it might engage any of the other senses.
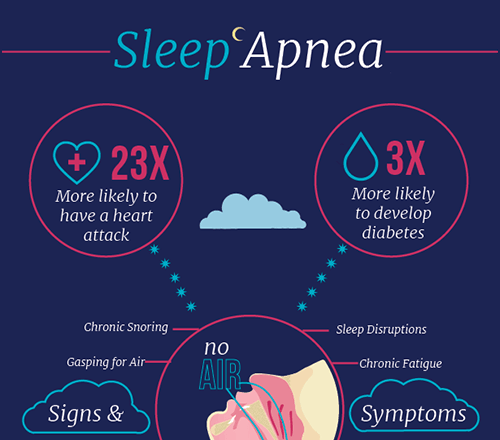
Insomnia and fragmented sleep. While persons with narcolepsy are excessively tired throughout the day, they frequently have difficulty sleeping at night. Insomnia, intense dreaming, sleep apnea, acting out while dreaming, and frequent leg movements disrupt sleep.
What is the cause of narcolepsy?
Although the cause of narcolepsy is unknown, current research suggests that it may result from a combination of circumstances contributing to a hypocretin deficiency. These factors include the following:
Disorders of the auto-immune system. When cataplexy occurs, the most common reason is the death of hypocretin-producing brain cells. Although the cause of this cell loss is uncertain, it appears to be related to immune system disorders. Autoimmune illnesses occur when the body’s immune system malfunctions and targets healthy cells or tissue inadvertently. According to researchers, persons with narcolepsy have an immune system that targets hypocretin-containing brain cells selectively due to a combination of hereditary and environmental variables.
Ancestral history. The majority of occurrences of narcolepsy are sporadic, meaning they occur in individuals who have no known family history of the illness. However, familial clusters do occurup to 10% of people diagnosed with narcolepsy with cataplexy report having a close cousin who exhibits comparable symptoms.
Trauma to the brain. Narcolepsy can occur due to acute injury to the brain regions that govern wakefulness and REM sleep, or as a result of tumors and other disorders in those regions.
Narcolepsy is diagnosed in a variety of ways.
A clinical examination and a thorough medical history requires for narcolepsy diagnosis and therapy. Their doctor may ask individuals to keep a sleep journal for one to two weeks, noting their sleep patterns and symptoms. While none of the principal symptoms are unique to narcolepsy, cataplexy is the most distinctive symptom, occurring in nearly no other condition.
Polysomnographic examination (PSG or sleep study). The PSG is a continuous recording of brain and muscle activity, respiration, and eye movements over an extended period. A PSG can assist in determining whether REM sleep occurs early in the sleep cycle and whether an individual’s symptoms causes by another disorder, such as sleep apnea.
Multiple sleep deprivation test (MSLT). The MSLT evaluates daytime drowsiness by determining how soon an individual falls asleep and if they enter REM sleep. On the PSG day, an individual asks to take five brief naps separated by two hours. If an individual sleeps for less than eight minutes on average during the five naps, this indicates excessive daytime sleepiness. However, individuals with narcolepsy also have an abnormally rapid onset of REM sleep. If REM sleep occurs within 15 minutes at least twice during the five naps and the previous night’s sleep study, this is most certainly a narcolepsy-related anomaly.
At times, measuring the level of hypocretin in the fluid that surrounds the brain and spinal cord may be beneficial. A doctor will use a lumbar puncture (sometimes called a spinal tap) to get a sample of the cerebrospinal fluid and measure the level of hypocretin-1. Low hypocretin-1 levels nearly often indicate type 1 narcolepsy in the absence of any significant medical issues.
What are the available treatments?
Take brief naps. Many people take a brief, timed naps at times when they are most sleepy.
Maintain a consistent sleeping routine. Even on weekends, going to bed and waking up simultaneously each day can help people sleep better.
Avoid caffeine and alcohol before going to bed. Individuals should abstain from alcohol and caffeine many hours before going to bed.
Avoid smoking at all costs , particularly at night.
Daily exercise is necessary. Exercising for at least 20 minutes each day, at least four or five hours before bedtime, improves sleep quality and may help persons with narcolepsy prevent weight gain.
Avoid large, heavy meals before going to bed. Consuming food too close to bedtime can make sleeping more difficult.
Before going to bed, unwind. Before bedtime, relaxing activities such as a warm bath might assist in encouraging sleepiness. Additionally, ensure that the sleeping area is cool and comfy.