Insulin: The Effect on the Body
Author: Alvin
Alvin
Category: Fitness

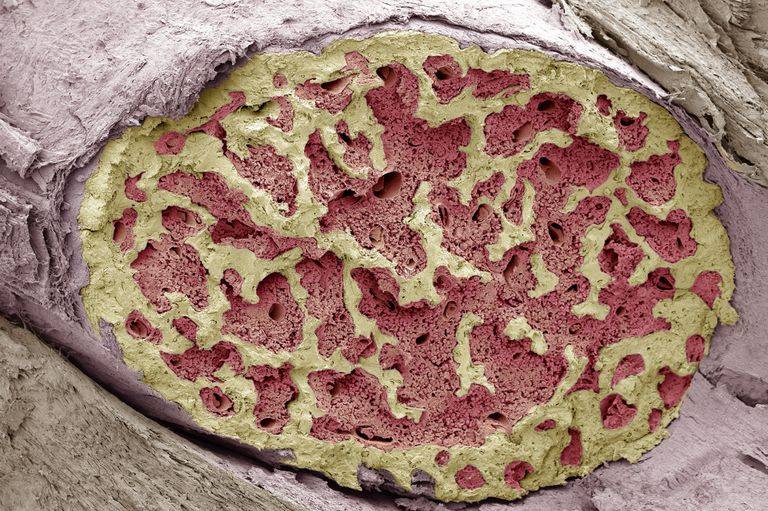
Insulin is a messenger chemical that enables cells to take up glucose, a sugar, from the blood.
The pancreas is a part of the digestive system behind the stomach that produces insulin as the body’s primary source. The cells that comprise the clusters of islets within the pancreas are known as islets, and they make the hormone that governs blood glucose levels.
A higher level of glucose is required to stimulate insulin release, which helps regulate blood sugar levels.
In addition to supporting glucose absorption, insulin also breaks down fats and proteins for energy.
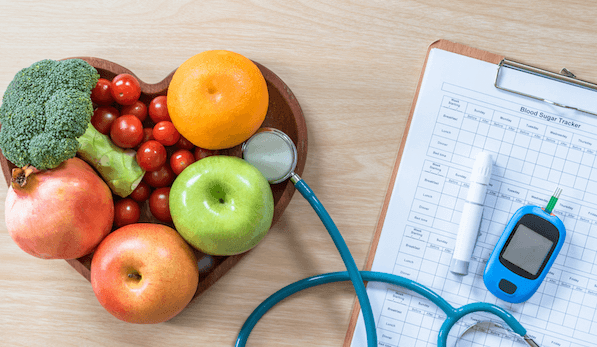
Insulin regulates the glucose levels in the blood and many other body processes. If an unstable or consistently high blood sugar state persists, serious medical problems may begin to emerge.
The Importance of Insulin
Insulin is a hormone that produces in your pancreas, a gland located behind your stomach. It provides your body with the ability to use glucose for energy. Glycogen is a carbohydrate with which many carbohydrates contain glucose.
Carbohydrates after a meal or snack are broken down in the digestive tract and changed into glucose. When glucose enters your bloodstream through the lining in your small intestine, it absorbs into your body. Once your blood glucose levels elevate, insulin promotes the cells in your body to absorb the sugar and convert it into energy.
It is also an essential factor in keeping your blood glucose levels balanced. Insulin signals your body to store glucose in your liver when too much of it is in your bloodstream. The stored glucose gets released only when your blood glucose levels fall, such as when you have eaten or when your body is stressed or needs a boost of energy.
Insulin as Treatment
Both types of diabetes can be treated with insulin injections. This artificial serves as a supplement to the natural insulin your body produces. Without producing insulin, people with type 1 diabetes must rely on injections to manage their blood glucose levels.
Type 2 diabetes is treatable with lifestyle changes and oral medication, and many people have learned to control their blood glucose levels this way.
Types of Treatment
Regardless of which type of one uses, the result is the same. The levels in the body go up and down naturally throughout the day. When it comes to the makeup of different types of insulin, how long and how quickly each of them works depends.
Rapid-acting: It administered via subcutaneous injection will take effect after approximately 15 minutes. The impact of its effects can last anywhere from three to four hours. It consumes before meals.
Short-acting: After you give it an injection, it begins working in about 30 to 60 minutes and lasts five to eight hours.
Intermediate-acting: It takes between one to two hours for this type to start working, and its effects may last for around 14 to 16 hours.
Long-acting: When injected, this may not be effective for at least two hours. As long as the individual expose to the substance, its effects can last 24 hours or longer.
Talk to your doctor
It is an essential medicine that aids in the maintenance of a healthy blood glucose level when appropriately used. If you have diabetes, it’s essential to monitor your blood glucose levels regularly.
And consult with your doctor about strategies that can help you maximize the effects of your treatment.
How are you going to take your insulin?
Many people with diabetes who self-administer do so via syringe injection. The syringe’s exterior mark with lines indicating the amount of medication contained in the needle. With the assistance of your doctor, you can select from a variety of syringe sizes.
How are you going to take?
Many people with diabetes who self-administer insulin do so via syringe injection. The syringe’s exterior mark with lines indicating the amount of medication contained in the needle. With the assistance of your doctor, you can select from a variety of syringe sizes.
How do you choose the correct insulin syringe?
If your highest dose is close to the maximum capacity of the syringe, consider purchasing the next size up in case your dosage increases.
If you measure your doses in half units, take care to select a syringe with the appropriate measurements.
When traveling, ensure that you purchase the correct size syringe for your insulin strength if you purchase new syringes in an unfamiliar location.
As with syringes, needles come in a variety of sizes. Generally, shorter needles result in less stinging when injecting. The disadvantage is that the shallower the injection, the longer takes to work. Your physician will assist you in achieving the optimal balance for you.
How do you administer insulin in the absence of a syringe?
Pens resemble large writing pens and can aid in the prevention of both under- and overdosing. Additionally, they do not require refrigeration, are more convenient than syringes and are more durable.
Insulin pumps connect to a thin tube implanted beneath the skin. Automatic or motorized pumps are available, and some models double as glucose monitors. They deliver insulin before each meal and in small doses throughout the day. Around 60% of people with diabetes in the United States use some form of the insulin pump.
If you despise needles, jet injection devices are an excellent alternative. A jet injector is a device that holds multiple doses of insulin. After pressing it against your skin, the insulin pushes through.
Because it is short-acting and is typically not covered by insurance, it is more expensive than other insulin types for most people with diabetes.
Unless you have a dual-function insulin pump and glucose monitor, insulin dosing is determined by self-monitoring your blood glucose levels. You can monitor them by performing finger pricks or by wearing a device that does the monitoring for you.
What is the best way to store?
Maintain at room temperature (a few days or a week’s supply) to help alleviate injection discomfort.
Insulin is typically stable at room temperature for approximately one month. Insulin pen expiration dates vary according to the type of insulin used. When using disposable pens, you should discard the entire device when it is empty or when the expiration date has passed.
Refrigerate any excess insulin (e.g., a two-three-week supply or more).
Insulin should not expose to extremes of cold or heat. (Avoid freezing or storing it in direct sunlight.)
What are non-insulin medications available to people with diabetes?
Metformin - a medication that prevents the liver from producing sugar
Glitazones - medicines that assist in the removal of sugar from the bloodstream
Sulfonylureas and glinides - medications that stimulate the pancreas’s release of insulin
Starch blockers - pills that inhibit the absorption of starch
Incretin therapies and amylin analogs - pills and injections suppress the liver’s sugar production and slow food digestion. DPP4 inhibitors (such as Januvia) and GLP1 analogs are examples of the former (like Victoza).
SGLT2 inhibitors - pills taken before meals that prevent glucose reabsorption
What additional measures can I take to maintain a healthy blood glucose
level?
Food, sleep, and exercise are all critical components of diabetes management.
Get adequate sleep. Endocrinologist Al Powers MD of Vanderbilt University, notes that when people are deprived of sleep or have their sleep disrupted, their glucose levels tend to rise, whether or not they have diabetes.
Exercise regularly. Insulin sensitivity increases during exercise, and muscle cells utilize available insulin more efficiently. While exercising, your muscles absorb glucose and use it for energy.
Adhere to a diabetic-safe diet with a low carbohydrate count, such as the DASH diet or the Mediterranean diet, as recommended by your doctor.