Heart Arrhythmia: Symptoms, Causes, and Types
Author: Giselle Robel
Giselle Robel
Category: Health
Tags: health, arrhythmia, heart, blood
Heart Arrhythmia or heart rhythm problems occur when the electrical impulses that coordinate your heartbeats don’t work properly, causing your heart to beat too fast, too slow, or irregularly.
It may feel like a fluttering or racing heart and may be harmless. However, some heart arrhythmias may cause bothersome sometimes even life-threatening signs and symptoms.
Heart arrhythmia treatment can often control or eliminate fast, slow or irregular heartbeats. And in addition to that, heart arrhythmias can be troublesome and are often made worse or are even caused by a weak or damaged heart, you may be able to reduce your arrhythmia risk by adopting a heart- healthy lifestyle.
What is a Heart Arrhythmia?
Heart arrhythmia refers to a group of conditions that cause the heart to beat irregularly, too slowly, or too quickly.
There are several categories of arrhythmia, including:
- bradycardia, or a slow heartbeat
- tachycardia, or a fast heartbeat
- irregular heartbeat, also known as a flutter or fibrillation
- early heartbeat, or a premature contraction
Most arrhythmias are not severe and do not cause complications. However, some can increase the risk of stroke or cardiac arrest.
Some people may hear doctors use the word dysrhythmia when referring to their irregular heartbeat. However, the words arrhythmia and dysrhythmia mean the same, but the word arrhythmia is more prevalent.
Understading the Heart
The heart is made up of four chambers two upper chambers (atrium) and two lower chambers (ventricles). Your heart rhythm is normally controlled by a natural pacemaker (sinus node) located in the right atrium. The sinus node produces electrical impulses that normally start each heartbeat. These impulses cause the atria muscles to contract and pump blood into the ventricles.

The top chambers of the heart are called the left atrium and right atrium. The bottom chambers of the heart are the left ventricle and right ventricle, which have thicker walls.
- The right atrium receives blood from the veins that has already circulated through the body and pumps it over to the right ventricle.
- The right ventricle passes the blood on to the pulmonary artery, which sends it to the lungs to pick up oxygen.
- The left atrium receives the now oxygen-rich blood from the lungs and pumps it into the left ventricle.
- The left ventricle pumps the oxygen-rich blood to the body through a large network of arteries. The contractions of the left ventricle, the strongest of the four chambers, are what creates blood pressure in the body.
A normal heartbeat is
Doctors identify a healthy heartbeat by counting the number of times the heart beats every minute (bpm) during rest. And this is known as the resting heart rate.
However, the range for a healthy resting heart rate varies between individuals, but the American Heart Association (AHA) suggests that it is usually between 60 and 100 bpm.
The fitter a person is, the lower their resting heart rate becomes.
The heart should beat with a regular rhythm, consisting of double ba-bum beats with even spaces in between each.
One of these beats is the heart contracting to provide oxygen to the blood that has already circulated, and the other involves the heart pushing oxygenated blood around the body.
A person can measure their heart rate using their pulse. This is a point at which they can feel the heartbeat through the skin. The best locations on the body for this are:
- the wrists
- the insides of the elbows
- the side of the neck
- the top of the foot
Types
There are several types of arrhythmia, as described here:
Atrial fibrillation
This is the irregular beating of the atrial chambers, and nearly always involves tachycardia. Atrial fibrillation (A-fib) is common and mainly develops in adults over 65 years of age.
Instead of producing a single, strong contraction, the chamber fibrillates, or quivers, often producing a rapid heartbeat.
Atrial flutter
While fibrillation causes many random and different quivers in the atrium, atrial flutter is usually from one area in the atrium that is not conducting properly. This produces a consistent pattern in the abnormal heart conduction.
Some people may experience both flutter and fibrillation.
Atrial flutter can be a serious condition and usually leads to fibrillation without treatment.
Supraventricular tachycardia
The condition known as supraventricular tachycardia (SVT) refers to a rapid but rhythmically regular heartbeat. An individual can experience a burst of accelerated heartbeats that can last from a few seconds to a few hours.
Doctors classify atrial fibrillation and flutter under SVTs.
Ventricular tachycardia
Ventricular tachycardia is a rapid, regular heart rate that originates with abnormal electrical signals in the ventricles.
The rapid heart rate doesn’t allow the ventricles to fill and contract efficiently to pump enough blood to the body.
Ventricular tachycardia may not cause serious problems if you have an otherwise healthy heart, but it can be a medical emergency that requires prompt medical treatment if you have heart disease or a weak heart.
This condition refers to abnormal electrical impulses that start in the ventricles and cause an abnormally fast heartbeat. This often happens if the heart has a scar from a previous heart attack.
Ventricular fibrillation
Ventricular fibrillation occurs when rapid, chaotic electrical impulses cause the ventricles to quiver ineffectively instead of pumping necessary blood to the body. This serious problem is fatal if the heart isn’t restored to a normal rhythm within minutes.
Most people who experience ventricular fibrillation have underlying heart disease or have experienced serious trauma.
This is an irregular heart rhythm consisting of rapid, uncoordinated, and fluttering contractions of the ventricles. The ventricles do not pump blood but quiver instead.
Ventricular fibrillation can be life-threatening and usually has links to heart disease. A heart attack often triggers it.
Wolff-Parkinson-White syndrome
In Wolff-Parkinson-White syndrome, a type of supraventricular tachycardia, there is an extra electrical pathway between the atria and the ventricles, which is present at birth. However, you may not experience symptoms until you’re an adult. This pathway may allow electrical signals to pass between the atria and the ventricles without passing through the AV node, leading to short circuits and rapid heartbeats.
Long QT syndrome
Long QT syndrome is a heart disorder that carries an increased risk of fast, chaotic heartbeats. The rapid heartbeats, caused by changes in the electrical system of your heart, may lead to fainting and can be life-threatening. And, in some cases, your heart’s rhythm may be so erratic that it can cause sudden death.
You can be born with a genetic mutation that puts you at risk of long QT syndrome. In addition, several medications may cause long QT syndrome. Some medical conditions, such as congenital heart defects, may also cause long QT syndrome.
Premature heartbeats
Although it often feels like a skipped heartbeat, a premature heartbeat is actually an extra beat. Even though you may feel an occasional premature beat, it seldom means you have a more serious problem. Still, a premature beat can trigger a long-lasting arrhythmia especially in people with heart disease. Frequent premature beats that last for several years may lead to a weak heart.
Premature heartbeats may occur when you’re resting or may sometimes be caused by stress, strenuous exercise or stimulants, such as caffeine or nicotine.
Bradycardia A slow heartbeat
Although a heart rate below 60 beats a minute while at rest is considered bradycardia, a low resting heart rate doesn’t always signal a problem. If you’re physically fit, you may have an efficient heart capable of pumping an adequate supply of blood with fewer than 60 beats a minute at rest.
In addition, certain medications used to treat other conditions, such as high blood pressure, may lower your heart rate. However, if you have a slow heart rate and your heart isn’t pumping enough blood, you may have one of several bradycardias, including:
- Sick sinus syndrome – If your sinus node, which is responsible for setting the pace of your heart, isn’t sending impulses properly, your heart rate may alternate between too slow (bradycardia) and too fast (tachycardia). This can also be caused by scarring near the sinus node that’s slowing, disrupting or blocking the travel of impulses. Sick sinus syndrome is most common among older adults.
- Conduction block – A block of your heart’s electrical pathways can occur in or near the AV node, which lies in the pathway between your atria and your ventricles. A block can also occur along other pathways to each ventricle.Depending on the location and type of block, the impulses between the upper and lower halves of your heart may be slowed or blocked. If the signal is completely blocked, certain cells in the AV node or ventricles can make a steady, although usually slower, heartbeat.Some blocks may cause no signs or symptoms, and others may cause skipped beats or bradycardia.
Symptoms
Arrhythmias may not cause any signs or symptoms.
In fact, your doctor might find you have arrhythmia before you do, during a routine examination. Noticeable signs and symptoms don’t necessarily mean you have a serious problem, however.
Noticeable arrhythmia symptoms may include:
- A fluttering in your chest
- A racing heartbeat (tachycardia)
- A slow heartbeat (bradycardia)
- Chest pain
- Shortness of breath
Other symptoms may include:
- Anxiety
- Fatigue
- Lightheadedness or dizziness
- Sweating
- Fainting (syncope) or near fainting
Causes
Certain conditions can lead to, or cause, an arrhythmia, including:
- A heart attack that’s occurring right now
- Scarring of heart tissue from a prior heart attack
- Changes to your heart’s structure, such as from cardiomyopathy
- Blocked arteries in your heart (coronary artery disease)
- High blood pressure
- Overactive thyroid gland (hyperthyroidism)
- Underactive thyroid gland (hypothyroidism)
- Diabetes
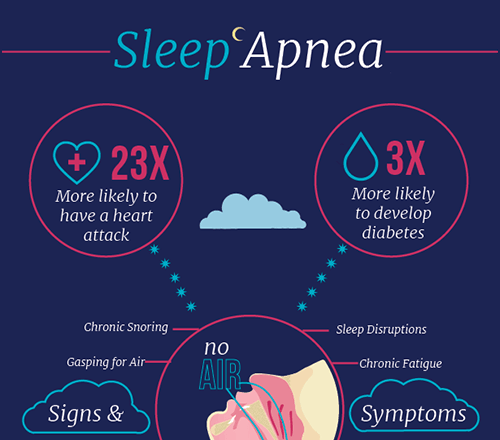
- Sleep apnea
- Infection with COVID-19
Other things that can cause an arrhythmia includes:
- Smoking
- Drinking too much alcohol or caffeine
- Drug abuse
- Stress or anxiety
- Certain medications and supplements, including over-the-counter cold and allergy drugs and nutritional supplements
- Genetics
Diagnosis
To diagnose an arrhythmia, a doctor has to identify the unusual heartbeat and try to find its source or trigger. This will involve a detailed interview, which may touch on medical history, family history, diet, and lifestyle.
Most importantly a doctor may request the following tests to support an arrhythmia diagnosis:
- blood and urine
- EKG
- A Holter monitor, a wearable device to record the heart for 1-2 days
- echocardiogram
- chest X-ray
- a tilt-table test to help identify if sudden decreases in blood pressure or heart rate are the cause
- electrophysiologic testing
- heart catheterization
Risk factors
Certain conditions may increase your risk of developing an arrhythmia. And these include the following:
- Coronary artery disease, other heart problems and previous heart surgery
- Narrowed heart arteries, a heart attack, abnormal heart valves, prior heart surgery, heart failure, cardiomyopathy and other heart damage are risk factors for almost any kind of arrhythmia.
- High blood pressure
- This increases your risk of developing coronary artery disease.
- It may also cause the walls of your left ventricle to become stiff and thick, which can change how electrical impulses travel through your heart.
- Congenital heart disease
- Being born with a heart abnormality may affect your heart’s rhythm.
- Thyroid problems
- Having an overactive or underactive thyroid gland can raise your risk of arrhythmias.
- Diabetes
- Your risk of developing coronary artery disease and high blood pressure greatly increases with uncontrolled diabetes.
- Obstructive sleep apnea
- This disorder, in which your breathing is interrupted during sleep, can increase your risk of bradycardia, atrial fibrillation and other arrhythmias.
- Electrolyte imbalance
- Substances in your blood called electrolytes such as potassium, sodium, calcium and magnesium help trigger and conduct the electrical impulses in your heart. Electrolyte levels that are too high or too low can affect your heart’s electrical impulses and contribute to arrhythmia development.
Other factors that may put you at higher risk of developing an arrhythmia include:
- Drugs and supplements
- Certain over-the-counter cough and cold medicines and certain prescription drugs may contribute to arrhythmia development.
- Drinking too much alcohol
- Drinking too much alcohol can affect the electrical impulses in your heart and can increase the chance of developing atrial fibrillation.
- Caffeine, nicotine or illegal drug use
- Caffeine, nicotine and other stimulants can cause your heart to beat faster and may contribute to the development of more-serious arrhythmias.
- Illegal drugs, such as amphetamines and cocaine, may profoundly affect the heart and lead to many types of arrhythmias or to sudden death due to ventricular fibrillation.
Complications
Certain arrhythmias may increase your risk of developing conditions such as:
- Stroke
- Heart arrhythmias are associated with an increased risk of blood clots. And if a clot breaks loose, it can travel from your heart to your brain.
- There it might block blood flow, causing a stroke. If you have a heart arrhythmia, your risk of stroke is increased if you have an existing heart disease or are 65 or older.
- And also certain medications, such as blood thinners, can greatly lower your risk of stroke or damage to other organs caused by blood clots.
- Heart failure
- And in addition a heart failure can result if your heart is pumping ineffectively for a prolonged period due to a bradycardia or tachycardia, such as atrial fibrillation.
- Sometimes controlling the rate of an arrhythmia that’s causing heart failure can improve your heart’s function.
Prevention
To prevent heart arrhythmia, it’s important to live a heart-healthy lifestyle to reduce your risk of heart disease. A heart-healthy lifestyle may include:
- Eating a heart-healthy diet
- Staying physically active and keeping a healthy weight
- Avoiding smoking
- Limiting or avoiding caffeine and alcohol
- Reducing stress, as intense stress and anger can cause heart rhythm problems
- Using over-the-counter medications with caution, as some cold and cough medications contain stimulants that may trigger a rapid heartbeat
Treatments
Treatment for arrhythmia is only necessary if the condition is increasing the risk of more severe arrhythmia or a complication, or if the symptoms are severe.
The various arrhythmias require different treatments.
Treatments for bradycardia
If bradycardia occurs due to an underlying condition, a doctor will need to treat that condition first.
If they find no underlying problem, the doctor may advise implanting a pacemaker.
A pacemaker is an implantable device that helps control abnormal heart rhythms.
A small device is placed under the skin near the collarbone in a minor surgical procedure.
An insulated wire extends from the device to the heart, where it’s permanently anchored.
If a pacemaker detects a heart rate that’s abnormal, it emits electrical impulses that stimulate your heart to beat at a normal rate.
Treatments for tachycardia
There are several different treatments for tachycardia:
Medications
These will not cure an arrhythmia, but are usually effective in reducing the number of tachycardia episodes.
Vagal maneuvers
Specific movements and exercises that a person can carry out at home might stop some types of arrhythmia that start above the lower half of the heart.
Additional treatment
Cardioversion
The doctor may use an electric shock or medication to reset the heart to its regular rhythm.
Ablation therapy
A surgeon inserts one or more catheters into the inner heart.
They place the catheters in areas of the heart that they suspect may be the source of the arrhythmia.
The surgeon will then use them to destroy small sections of damaged tissue, which often corrects the arrhythmia.
Implantable cardioverter-defibrillator (ICD)
Your doctor may recommend this device if you’re at high risk of developing a dangerously fast or irregular heartbeat in the lower half of your heart (ventricular tachycardia or ventricular fibrillation).
And if you have had a sudden cardiac arrest or have certain heart conditions that increase your risk of sudden cardiac arrest, your doctor may also recommend an ICD.
An ICD is a battery-powered unit that’s implanted under the skin near the collarbone similar to a pacemaker.
One or more electrode-tipped wires from the ICD run through the veins to the heart.
The ICD continuously monitors your heart rhythm.
If it detects an abnormal heart rhythm, it sends out low- or high-energy shocks to reset the heart to a normal rhythm.
An ICD doesn’t prevent an abnormal heart rhythm from occurring, but it treats it if it occurs.
If it detects an unusually fast rate, it stimulates the heart to return to its normal speed.
Maze procedure
During the maze procedure, a surgeon makes a series of surgical incisions in the heart.
These then turn into scars and form blocks that guide the electrical impulses, helping the heart to beat efficiently.
Ventricular aneurysm surgery
Sometimes, an aneurysm, or bulge, in a blood vessel that leads to the heart can cause arrhythmia.
If other treatments are not effective, a surgeon may have to remove the aneurysm.
Coronary bypass surgery
A surgeon grafts arteries or veins from elsewhere in the body and into the coronary arteries.
This helps the circulation bypass any regions that have become narrow and improves the blood supply to the heart muscle.