Uterine Cancer
Author: Shiela Lupiba
Shiela Lupiba
Category: Health
Tags: health, uterine, uterus, women's health, cancer

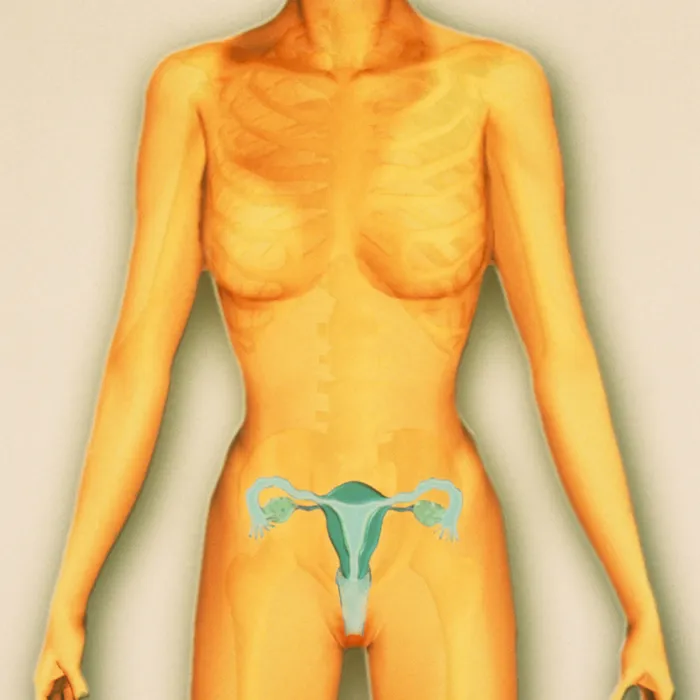
Uterine cancers can be of two types: endometrial cancer (common) and uterine sarcoma (rare). Endometrial cancer can often be cured. Uterine sarcoma is often more aggressive and harder to treat.
Also, it typically develops after menopause. Obese women are more likely to have it. You are also at a higher risk if you have been on estrogen-only hormone replacement therapy (menopausal hormone therapy) for a long time.
Endometrial Cancer
Endometrial cancer is cancer that starts in the uterus. The uterus is a hollow, pear-shaped pelvic organ in which fetal development takes place. It begins in the layer of cells that forms the uterine lining (endometrium).
Also, it is frequently detected at an early stage due to abnormal vaginal bleeding. When endometrial cancer is discovered early, surgically removing the uterus often cures it.
Uterine Sarcoma
Uterine sarcoma is a disease that causes malignant (cancer) cells to form in the uterine muscles or other tissues that support the uterus. Radiation therapy to the pelvis in the past can increase the risk of uterine sarcoma. Abnormal bleeding is one of the symptoms of uterine sarcoma.
Symptoms
If you have any of the following symptoms of endometrial cancer or uterine sarcoma, the two most common types of uterine cancer:
- Ignore Uterine Cancer Warning Signs such as vaginal bleeding or spotting. Because they consult their doctor about abnormal vaginal bleeding, approximately 67 percent of women are able to detect uterine cancer in its early stages.
- Vaginal discharge that is abnormal and may be bloody or non-bloody
- Any vaginal bleeding after menopause
- A palpable mass or tumor in your lower abdomen (belly).
- Pain in your lower abdomen or pelvic area (belly)
- Losing weight without making an effort
- Having difficulty or experiencing pain when urinating
- Pain during a sexual encounter
“If you have bleeding that is out of the ordinary for you, especially if you are past menopause,” says Michael S. Guy, MD of Premier Gynecologic Oncology. “Your doctor can assist you in determining whether the bleeding will cause by cancer or another condition that necessitates medical treatment.” Then you’ll know what you’re up against and can decide on the best next steps together.”
Causes
Although the exact causes of uterine cancer are unknown, risk factors include women with endometrial hyperplasia, obesity, women who have never had children, menstruation beginning before the age of 12, menopause after the age of 55, estrogen therapy, tamoxifen use, pelvic radiation, and a family history of uterine cancer.
Some factors that can increase your risk of uterine cancer include:
- being postmenopausal, or reaching menopause (after age 55)
- a thickened wall lining (endometrial hyperplasia)
- never having children
- starting periods early (before age 12)
- having high blood pressure or diabetes
- being overweight or obese
- family history of ovarian, uterine, or bowel cancer
- having a genetic condition such as Cowden syndrome or Lynch syndrome
- previous ovarian tumours, or polycystic ovary syndrome
- using oestrogen only hormone replacement therapy or fertility treatment
- previous radiation therapy to the pelvis
- taking tamoxifen to treat breast cancer (the benefits of treating breast cancer usually outweigh the risk of uterine cancer – (talk to your doctor if you are concerned).
Diagnosis
Many tests are used by doctors to detect or diagnose cancer. They perform tests to determine whether the cancer has spread to a different part of the body from where it began.
This section describes options for diagnosing uterine cancer.
- Examine the pelvis. The doctor examines the uterus, vagina, ovaries, and rectum for any abnormalities. A Pap test, which is frequently combine with a pelvic examination, is primarily use to screen for cervical cancer. A Pap test may occasionally reveal abnormal glandular cells caused by uterine cancer.
- Biopsy of the endometrium. A biopsy is the removal of a small amount of tissue for microscopic examination. Other tests can indicate the presence of cancer, but only a biopsy can provide a definitive diagnosis. The sample is examine by a pathologist (s). A pathologist is a doctor who specializes in interpreting laboratory tests and analyzing cell and tissue samples in order to diagnose disease.
- Transvaginal ultrasound. An ultrasound creates a picture of internal organs by using sound waves. An ultrasound wand inserts into the vagina and aimed at the uterus to take pictures during a transvaginal ultrasound. If the endometrium appears to be too thick, the doctor may decide to biopsy it.
- Magnetic resonance imaging (MRI) (MRI). An MRI produces detailed images of the body by using magnetic fields rather than x-rays. The tumor’s size can be determin using an MRI. To create a clearer image, a special dye called a contrast medium can be given intravenously or orally before the scan, as with a CT scan.
Uterine Cancer Stages and Treatments
 https://weillcornell.org/services/obstetrics-and-
gynecology/gynecologic-oncology/conditions-we-treat/endometrial-and-uterine-
cancer
https://weillcornell.org/services/obstetrics-and-
gynecology/gynecologic-oncology/conditions-we-treat/endometrial-and-uterine-
cancer
STAGE 1
The cancer has not spread beyond your uterus at this point. It may also affect the cervix glands (the narrow passage at the bottom of your uterus), but not the tissues. This stage includes the following elements:
Stage 1A: The cancer has spread to the endometrium, the inner lining of your
uterus. It could have spread only halfway into the underlying muscle.
Stage 1B: The cancer has spread to the endometrium and has progressed more
than halfway through the underlying muscle.
Treatment. The standard treatment is a total hysterectomy, which involves removing the uterus and cervix, as well as the fallopian tubes and ovaries.
STAGE 2
The cancer has spread from the uterus into the cervix tissue, but it has not yet grown outside of the uterus.
Treatment. In most cases, you will undergo radical hysterectomy surgery to remove your uterus, the tissues surrounding it, and the upper part of your vagina. Your fallopian tubes and ovaries may also be removed by the surgeon. Radiation therapy or vaginal brachytherapy may also be required.
STAGE 3
The cancer has spread to the ovaries, fallopian tubes, vaginal cavity, or lymph nodes. However, it has not affected your bladder or the rectum’s inner lining.
Stage lllA: Cancer has spread to the outer layer of your uterus, as well as the fallopian tubes and ovaries.
Treatment. If your doctor believes that surgery can remove the cancer, a surgeon may perform a total or radical hysterectomy and remove your fallopian tubes and ovaries.
STAGE 4
Cancer has spread to the bladder, rectum, or organs other than the uterus, such as the lungs.
Stage IVA cancer has spread to the bladder or rectum, as well as possibly
nearby lymph nodes.
Stage IVB: It can be found in the upper abdomen, the fat that supports your
lower abdomen (known as the omentum), or organs such as your lungs, liver, and
bones. It could have spread to the lymph nodes in the groin.