Cervical Cancer: You Need to Know About
Author: Giselle Robel
Giselle Robel
Category: Health

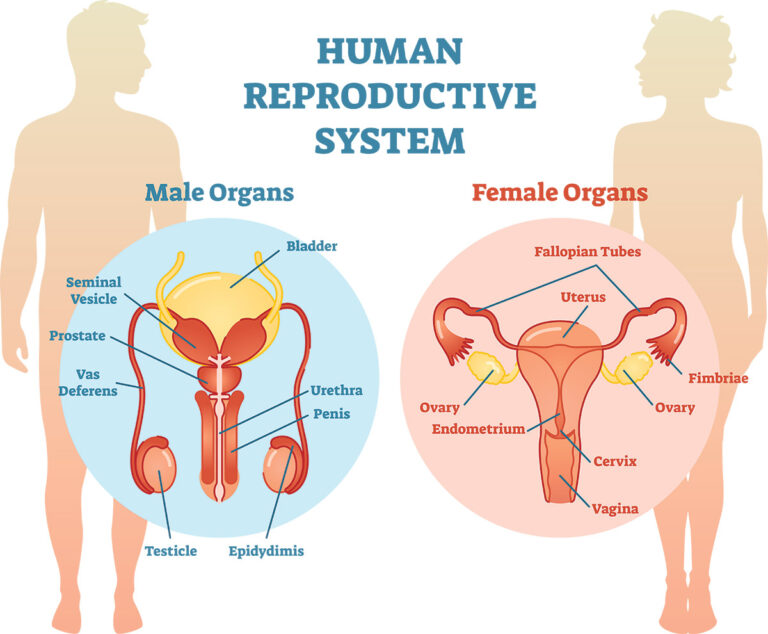
Cervical cancer is a type of cancer that starts in the cervix. The cervix is a hollow cylinder that connects the lower part of a woman's uterus to her vagina. Most cervical cancers begin in cells on the surface of the cervix.
Cervical cancer is a type of cancer that occurs in the cells of the cervix the lower part of the uterus that connects to the vagina.
Various strains of the human papillomavirus (HPV), a sexually transmitted infection, play a role in causing most cervical cancer.
When exposed to HPV, the body’s immune system typically prevents the virus from doing harm. In a small percentage of people, however, the virus survives for years, contributing to the process that causes some cervical cells to become cancer cells.
You can reduce your risk of developing cervical cancer by having screening tests and receiving a vaccine that protects against HPV infection.

Cervical Cancer Symptoms
Many women with cervical cancer don't realize they have the disease early on, because it usually doesn't cause symptoms until the late stages. When symptoms do appear, they're easily mistaken for common conditions like menstrual periods and urinary tract infections (UTIs).
Typical symptoms are:
- unusual bleeding, such as in between periods, after sex, or after menopause
- vaginal discharge that looks or smells different than usual
- pain in the pelvis
- needing to urinate more often
- pain during urination
Causes
Cervical cancer begins when healthy cells in the cervix develop changes (mutations) in their DNA. A cell’s DNA contains the instructions that tell a cell what to do.
Healthy cells grow and multiply at a set rate, eventually dying at a set time. The mutations tell the cells to grow and multiply out of control, and they don’t die. The accumulating abnormal cells form a mass (tumor). Cancer cells invade nearby tissues and can break off from a tumor to spread (metastasize) elsewhere in the body.
It isn’t clear what causes it, but it’s certain that HPV plays a role. HPV is very common, and most people with the virus never develop cancer. This means other factors such as your environment or your lifestyle choices also determine whether you’ll develop cervical cancer.
Most cases are caused by the sexually transmitted human papillomavirus (HPV). This is the same virus that causes genital warts.
There are about 100 different strains of HPV. Only certain types cause cervical cancer. The two types that most commonly cause cancer are HPV-16 and HPV-18.
Being infected with a cancer-causing strain of HPV doesn't mean you'll get cervical cancer. Your immune system eliminates the vast majority of HPV infections, often within two years.
HPV can also cause other cancers in women and men. These include:
- vulvar cancer
- vaginal cancer
- penile cancer
- anal cancer
- rectal cancer
- throat cancer
HPV is a very common infection.
 Cervical cancer development image
Cervical cancer development image
Types of cervical cancer
The type of cervical cancer that you have helps determine your prognosis and treatment. The main types are:
- Squamous cell carcinoma. This is a type that begins in the thin, flat cells (squamous cells) lining the outer part of the cervix, which projects into the vagina. Most cervical cancers are squamous cell carcinomas.
- Adenocarcinoma. This type begins in the column-shaped glandular cells that line the cervical canal.
Sometimes, both types of cells are involved in cervical cancer. Very rarely, cancer occurs in other cells in the cervix.
Cervical cancer treatment
Cervical cancer is very treatable if you catch it early. The four main treatments are:
- surgery
- radiation therapy
- chemotherapy
- targeted therapy
Sometimes these treatments are combined to make them more effective.
Surgery
The purpose of surgery is to remove as much of the cancer as possible. Sometimes the doctor can remove just the area of the cervix that contains cancer cells. For cancer that's more widespread, surgery may involve removing the cervix and other organs in the pelvis.
Radiation therapy
Radiation kills cancer cells using high-energy X-ray beams. It can be delivered through a machine outside the body. It can also be delivered from inside the body using a metal tube placed in the uterus or vagina.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells throughout the body. Doctors give this treatment in cycles. You'll get chemo for a period of time. You'll then stop the treatment to give your body time to recover.
Targeted therapy
Bevacizumab (Avastin) is a newer drug that works in a different way from chemotherapy and radiation. It blocks the growth of new blood vessels that help the cancer grow and survive. This drug is often given together with chemotherapy.
Risk factors
Risk factors include:
- Many sexual partners. The greater your number of sexual partners and the greater your partner’s number of sexual partners the greater your chance of acquiring HPV.
- Early sexual activity. Having sex at an early age increases your risk of HPV.
- Other sexually transmitted infections (STIs). Having other STIs such as chlamydia, gonorrhea, syphilis and HIV/AIDS increases your risk of HPV.
- A weakened immune system – You may be more likely to develop this kind of cancer if your immune system is weakened by another health condition and you have HPV.
- Smoking – Smoking increases the cervical cancer because of squamous cell.
- Exposure to miscarriage prevention drug. If your mother took a drug called diethylstilbestrol (DES) while pregnant in the 1950s, you may have an increased risk of a certain type of cervical cancer called clear cell adenocarcinoma.
Prevention
To reduce your risk:
- Ask your doctor about the HPV vaccine – Receiving a vaccination to prevent HPV infection may reduce your risk of cervical cancer and other HPV-related cancers. Ask your doctor whether an HPV vaccine is appropriate for you.
- Have routine Pap tests – Pap tests can detect precancerous conditions of the cervix, so they can be monitored or treated in order to prevent cervical cancer. Most medical organizations suggest beginning routine Pap tests at age 21 and repeating them every few years.
- Practice safe sex – Reduce your risk of cervical cancer by taking measures to prevent sexually transmitted infections, such as using a condom every time you have sex and limiting the number of sexual partners you have.
- Don’t smoke – If you don’t smoke, don’t start. If you do smoke, talk to your doctor about strategies to help you quit.
*[ HPV]: human papillomavirus