Tuberculosis: Symptoms, Causes, and Treatment
Author: Giselle Robel
Giselle Robel
Category: Health
Tags: health, bacteria, tuberculosis, tb

What is tuberculosis?
Tuberculosis (TB) is an infectious disease that mostly affects the lungs. But can also affect body parts like the spine, brain, or kidneys. However, not everyone who is infected gets sick. If you do get sick, you need treatment.
Tuberculosis (TB) is an infectious disease that mostly affects the lungs, but can also affect other parts of the body. Symptoms include a bad cough, pain in the chest, and coughing up blood.
It is a potentially serious infectious disease that mainly affects the lungs. The bacteria that cause tuberculosis are spread from person to person through tiny droplets released into the air via coughs and sneezes.
Once rare in developed countries, tuberculosis, infections began increasing in 1985, partly because of the emergence of HIV, the virus that causes AIDS. HIV weakens a person’s immune system, so it can’t fight TB germs. In the United States, because of stronger control programs, tuberculosis began to decrease again in 1993. But it remains a concern.
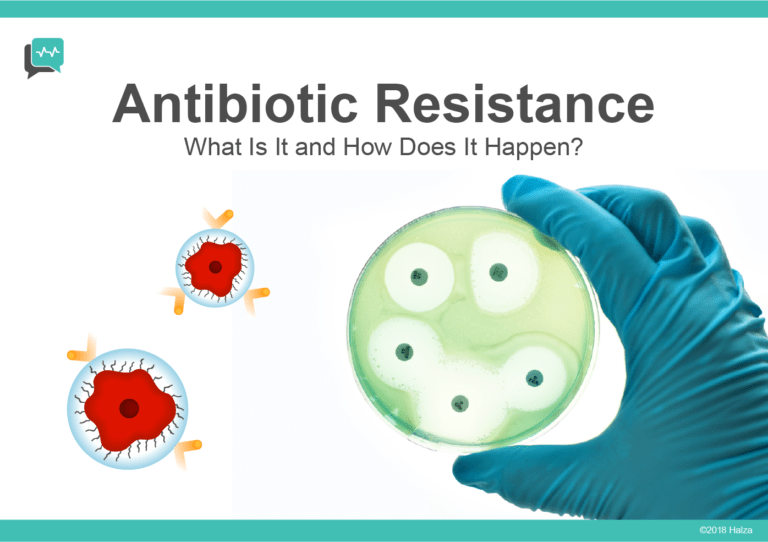
Many tuberculosis strains resist the drugs most used to treat the disease. People with active tuberculosis must take many types of medications for months to get rid of the infection and prevent antibiotic resistance.
Symptoms
Although your body can harbor the bacteria that cause tuberculosis, your immune system usually can prevent you from becoming sick. For this reason, doctors make a distinction between:
- Latent TB. You have a TB infection, but the bacteria in your body are inactive and cause no symptoms. Latent TB, also called inactive TB or TB infection, isn’t contagious. Latent TB can turn into active TB, so treatment is important.
- Active TB. Also called TB disease, this condition makes you sick and, in most cases, can spread to others. It can occur weeks or years after infection with the TB bacteria.
Signs and symptoms of active TB include:
- Coughing for three or more weeks
- Coughing up blood or mucus
- Chest pain, or pain with breathing or coughing
- Unintentional weight loss
- Fatigue
- Fever
- Night sweats
- Chills
- Loss of appetite
Tuberculosis can also affect other parts of your body, including the kidneys, spine, or brain. When TB occurs outside your lungs, signs, and symptoms vary according to the organs involved. For example, tuberculosis of the spine might cause back pain, and tuberculosis in your kidneys might cause blood in your urine.
When to see a doctor
See your doctor if you have a fever, unexplained weight loss, drenching night sweats, or a persistent cough. These are often indications of TB, but can also result from other conditions. See your doctor if you think you’ve been exposed to TB.
People who have an increased risk of tuberculosis be screened for latent TB infection. This recommendation includes people who:
- Have HIV/AIDS
- Use IV drugs
- Are in contact with infected people
- Are from a country where TB is common, such as several countries in Latin America, Africa and Asia
- Live or work in areas where TB is common, such as prisons or nursing homes
- Work in health care and treat people with a high risk of TB
- Are children who are exposed to adults at risk of TB
What causes tuberculosis?
TB is caused by the bacterium Mycobacterium tuberculosis. The germs are spread through the air and usually infect the lungs, but can also infect other parts of the body. Although TB is infectious, it does not spread easily. You usually have to spend a lot of time in contact with someone who is contagious in order to catch it.
How tuberculosis spread

TB can be spread when a person with active TB disease releases germs into the air through coughing, sneezing, talking, singing, or even laughing. Only people with active pulmonary infection are contagious. Most people who breathe in TB bacteria are able to fight the bacteria and stop it from growing. The bacterium becomes inactive in these individuals and is referred to as a latent TB infection. Approximately 10 percent of the US population has a latent infection.
Although the bacteria are inactive, they still remain alive in the body and can become active later. Some people can have a latent TB infection for a lifetime, without it ever becoming active and developing into TB disease. However, TB can become active if the immune system becomes weakened and cannot stop the bacteria from growing. This is when the latent TB infection becomes TB disease.
Tests used to diagnose tuberculosis
There are two kinds of screening tests for TB: the Mantoux tuberculin skin test (TST) and the blood test, called the interferon-gamma release assay (IGRA).
For the TST, a healthcare provider will inject a small amount of a substance called purified protein derivative (PPD) under the skin of the forearm. After 2-3 days, the person must go back to the healthcare provider, who will look at the injection site. If the person has a TB infection, there will be a reddish lump.
For the IGRA, a healthcare provider will draw blood and send the sample to the lab.
Further tests to determine if an infection is active or if lungs are infected include the following:
- Tests of sputum and lung fluid
- X-rays
- Computed tomography (CT) scans
Can tuberculosis be cured?
Yes, TB can be cured, even in people with HIV infection. Drugs used to treat TB infection and disease include isoniazid (Hyzyd®), rifampin (Rifadin®), ethambutol (Myambutol®), pyrazinamide (Zinamide®), and a combination of isoniazid and rifapentine.
You must take all of the medication your doctor tells you to, or else not all of the bacteria will be killed. You will have to take these medications for as long as you are toldsometimes up to 9 months.
Drug-resistant TB
Tuberculosis also remains a major killer because of the increase in drug- resistant strains. Over time, some TB germs have developed the ability to survive despite medications. This is partly because people don’t take their drugs as directed or don’t complete the course of treatment.
Drug-resistant strains of tuberculosis emerge when an antibiotic fails to kill all of the bacteria it targets. The surviving bacteria become resistant to that drug and often other antibiotics as well. Some TB bacteria have developed resistance to the most commonly used treatments, such as isoniazid and rifampin (Rifadin, Rimactane).
Some TB strains have also developed resistance to drugs less commonly used in TB treatment, such as the antibiotics known as fluoroquinolones, and injectable medications including amikacin and capreomycin (Capastat). These medications are often used to treat infections that are resistant to the more commonly used drugs.
Risk factors
Anyone can get tuberculosis, but certain factors can increase your risk, including:
Weakened immune system
A healthy immune system often successfully fights TB bacteria. However, several conditions and medications can weaken your immune system, including:
- HIV/AIDS
- Diabetes
- Severe kidney disease
- Certain cancers
- Cancer treatment, such as chemotherapy
- Drugs to prevent rejection of transplanted organs
- Some drugs used to treat rheumatoid arthritis, Crohn’s disease and psoriasis
- Malnutrition or low body weight
- Very young or advanced age
Traveling or living in certain areas
There’s a higher risk of getting tuberculosis if you live in or emigrate from or travel to areas with high tuberculosis rates. Areas include:
- Africa
- Asia
- Eastern Europe
- Russia
- Latin America
Other factors
- Using substances. IV drugs or excessive alcohol use weakens your immune system and makes you more vulnerable to tuberculosis.
- Using tobacco. Tobacco use greatly increases the risk of getting TB and dying of it.
- Working in health care. In regular contact with people who are ill increases your chances of exposure to TB bacteria. Wearing a mask and frequent handwashing greatly reduce your risk.
- Living or working in a residential care facility. People who live or work in prisons, homeless shelters, psychiatric hospitals or nursing homes are all at a higher risk of tuberculosis due to overcrowding and poor ventilation.
- Living with someone infected with TB. Close contact with someone who has TB increases your risk.
Complications
Not treating, tuberculosis can be fatal. The untreated active disease typically affects your lungs, but it can affect other parts of your body, as well.
Tuberculosis complications include:
- Spinal pain. Back pain and stiffness are common complications of tuberculosis.
- Joint damage. Arthritis that results from tuberculosis (tuberculous arthritis) usually affects the hips and knees.
- Swelling of the membranes that cover your brain (meningitis). This can cause a lasting or intermittent headache that occurs for weeks and possible mental changes.
- Liver or kidney problems. Your liver and kidneys help filter waste and impurities from your bloodstream. Tuberculosis in these organs can impair their functions.
- Heart disorders. Rarely, tuberculosis can infect the tissues that surround your heart, causing inflammation and fluid collections that might interfere with your heart’s ability to pump effectively. This condition, called cardiac tamponade, can be fatal.
Prevention
If you test positive for latent TB infection, your doctor might advise you to take medications to reduce your risk of developing active tuberculosis. Only active TB is contagious.
Protect your family and friends
If you have active TB, it generally takes a few weeks of treatment with TB medications before you’re not contagious anymore. Follow these tips to help keep your friends and family from getting sick:
- Stay home. Don’t go to work or school or sleep in a room with other people during the first few weeks of treatment.
- Ventilate the room. Tuberculosis germs spread more easily in small closed spaces where air doesn’t move. If it’s not too cold outdoors, open the windows and use a fan to blow indoor air outside.
- Cover your mouth. Use a tissue to cover your mouth anytime you laugh, sneeze or cough. Put the dirty tissue in a bag, seal it and throw it away.
- Wear a face mask. Wearing a face mask when you’re around other people during the first three weeks of treatment may help lessen the risk of transmission.
Finish your medication
This is the most important step you can take to protect yourself and others from tuberculosis. When you stop treatment early or skip doses, TB bacteria have a chance to develop mutations that allow them to survive the most potent TB drugs. The resulting drug-resistant strains are deadlier and more difficult to treat.
Vaccinations
In countries where tuberculosis is more common, infants often are vaccinated with bacille Calmette-Guerin (BCG) vaccine.
*[ TB]: tuberculosis