Pneumonia Symptoms and Diagnosis
Author: Giselle Robel
Giselle Robel
Category: Health
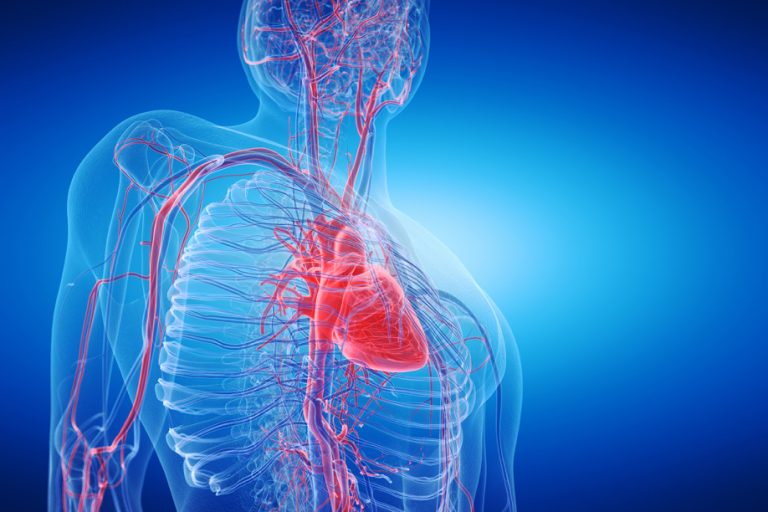
Pneumonia is an infection that inflames the air sacs in one or both lungs. Not only the air sacs may be filled with fluid or pus (purulent material), causing cough with phlegm or pus, fever, chills, and difficulty breathing. But also a variety of organisms, including bacteria, viruses, and fungi, can cause pneumonia.
Pneumonia can range in seriousness from mild to life-threatening. And it is more serious for infants and young children, people older than age 65, and people with health problems or weakened immune systems.
Symptoms of Pneumonia
Signs and symptoms of pneumonia vary from mild to severe. And also depending on factors such as the type of germ causing the infection, and your age, and overall health. Moreover, mild signs and symptoms are often similar to those of a cold or flu, but they last longer.
- Chest pain when you breathe or cough
- Confusion or changes in mental awareness (in adults age 65 and older)
- Cough, which may produce phlegm
- Fatigue
- Fever, sweating and shaking chills
- Lower than normal body temperature (in adults older than age 65 and people with weak immune systems)
- Nausea, vomiting or diarrhea
- Shortness of breath
Newborns and infants may not show any sign of the infection. However, they may vomit, have a fever and cough, appear restless or tired and without energy, or have difficulty breathing and eating.
More Additional Symptoms
Bacterial pneumonia, which is the most common form, tends to be more serious than other types of pneumonia, with symptoms that require medical care. In addition to that, the symptoms of bacterial pneumonia can develop gradually or suddenly. Fever may rise as high as a dangerous 105 degrees F, with profuse sweating and rapidly increased breathing and pulse rate. Lips and nail beds may have a bluish color due to a lack of oxygen in the blood. A patient’s mental state may be confused or delirious.
The symptoms of viral pneumonia usually develop over a period of several days. Early symptoms are similar to influenza symptoms: fever, a dry cough, headache, muscle pain, and weakness. Within a day or two, the symptoms typically get worse, with increasing cough, shortness of breath, and muscle pain. There may be a high fever and there may be blueness of the lips.
Many germs can cause pneumonia. The most common are bacteria and viruses in the air we breathe. Your body usually prevents these germs from infecting your lungs. But sometimes these germs can overpower your immune system, even if your health is generally good.
It is classified according to the types of germs that cause it and where you got the infection.
Community-acquired pneumonia
Community-acquired pneumonia is the most common type of pneumonia. It occurs outside of hospitals or other health care facilities. It may be caused by:
- Bacteria. The most common cause of bacterial pneumonia in the U.S. Is Streptococcus pneumoniae. This type of pneumonia can occur on its own or after you’ve had a cold or the flu. It may affect one part (lobe) of the lung, a condition called lobar pneumonia.
- Bacteria-like organisms. Mycoplasma pneumoniae also can cause pneumonia. It typically produces milder symptoms than do other types of pneumonia. Walking pneumonia is its informal name, which typically isn’t severe enough to require bed rest.
- Fungi. This type of pneumonia is most common in people with chronic health problems or weakened immune systems, and people who have inhaled large doses of the organisms. The fungi that cause it can be found in soil or bird droppings and vary depending upon geographic location.
- Viruses, including COVID-19. Some of the viruses that cause colds and the flu can cause pneumonia. Viruses are the most common cause of pneumonia in children younger than 5 years. Viral pneumonia is usually mild. But in some cases it can become very serious. Coronavirus 2019 (COVID-19) may cause pneumonia, which can become severe.
Hospital-acquired pneumonia
Some people catch pneumonia during a hospital stay for another illness. Hospital-acquired pneumonia can be serious because the bacteria causing it may be more resistant to antibiotics and because the people who get it are already sick. People who are on breathing machines (ventilators), often used in intensive care units, are at higher risk of this type of pneumonia.
Health care-acquired pneumonia
Is a bacterial infection that occurs in people who live in long-term care facilities or who receive care in outpatient clinics, including kidney dialysis centers. Like hospital-acquired pneumonia, healthcare-acquired pneumonia can be caused by bacteria that are more resistant to antibiotics.
Aspiration pneumonia
Occurs when you inhale food, drink, vomit or saliva into your lungs. Aspiration is more likely if something disturbs your normal gag reflex, such as a brain injury or swallowing problem, or excessive use of alcohol or drugs.
How Is Pneumonia Diagnosed?
Sometimes pneumonia can be difficult to diagnose because the symptoms are so variable, and are often very similar to those seen in a cold or influenza. To diagnose pneumonia, and to try to identify the germ that is causing the illness, your doctor will ask questions about your medical history, do a physical exam, and run some tests.
Medical history
Your doctor will ask you questions about your signs and symptoms, and how and when they began. To help figure out if your infection is caused by bacteria, viruses or fungi, you may be asked some questions about possible exposures, such as:
- Any recent travel
- Your occupation
- Contact with animals
- Exposure to other sick people at home, work or school
- Whether you have recently had another illness
Physical exam
Your doctor will listen to your lungs with a stethoscope. If you have pneumonia, your lungs may make crackling, bubbling, and rumbling sounds when you inhale.
Diagnostic Tests
If your doctor suspects you may have pneumonia, they will probably recommend some tests to confirm the diagnosis and learn more about your infection. These may include:
- Blood tests to confirm the infection and to try to identify the germ that is causing your illness.
- Chest X-ray to look for the location and extent of inflammation in your lungs.
- Pulse oximetry to measure the oxygen level in your blood. Pneumonia can prevent your lungs from moving enough oxygen into your bloodstream.
- Sputum test on a sample of mucus (sputum) taken after a deep cough, to look for the source of the infection.
If you are hospitalized you are considered a high-risk patient. And the doctors may want to do some additional tests, including:
- CT scans of the chest to get a better view of the lungs and look for abscesses or other complications.
- Arterial blood gas test , to measure the amount of oxygen in a blood sample taken from an artery, usually in your wrist. This is more accurate than the simpler pulse oximetry.
- Pleural fluid culture , which removes a small amount of fluid from around the tissues that surround the lung, to analyze and identify bacteria causing the pneumonia.
- Bronchoscopy, a procedure used to look into the lungs’ airways. If you are hospitalized and your treatment is not working well, doctors may want to see whether something else is affecting your airways, such as a blockage. They may also take fluid samples or a biopsy of lung tissue.
How Is Pneumonia Treated?
When you get a pneumonia diagnosis, your doctor will work with you to develop a treatment plan. Treatment for pneumonia depends on the type of pneumonia you have, how sick you are feeling, your age, and whether you have other health conditions. The goals of treatment are to cure the infection and prevent complications. It is important to follow your treatment plan carefully until you are fully recovered.
Take any medications as prescribed by your doctor. If your pneumonia is caused by bacteria, you will be given an antibiotic. It is important to take all the antibiotic until it is gone, even though you will probably start to feel better in a couple of days. If you stop, you risk having the infection come back, and you increase the chances that the germs will be resistant to treatment in the future.
Typical antibiotics do not work against viruses. If you have viral pneumonia, your doctor may prescribe an antiviral medication to treat it. Sometimes, though, symptom management and rest are all that is needed.
Additional Treatment
Most people can manage their symptoms such as fever and cough at home by following these steps:
- Control your fever with aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs, such as ibuprofen or naproxen), or acetaminophen. DO NOT give aspirin to children.
- Drink plenty of fluids to help loosen secretions and bring up phlegm.
- Do not take cough medicines without first talking to your doctor. Coughing is one way your body works to get rid of an infection. If your cough is preventing you from getting the rest you need, ask your doctor about steps you can take to get relief.
- Drink warm beverages, take steamy baths and use a humidifier to help open your airways and ease your breathing.
- Stay away from smoke to let your lungs heal. This includes smoking, secondhand smoke and wood smoke. Talk to your doctor if you are a smoker and are having trouble staying smokefree while you recover. This would be a good time to think about quitting for good.
- Get lots of rest. You may need to stay in bed for a while. Get as much help as you can with meal preparation and household chores until you are feeling stronger. It is important not to overdo daily activities until you are fully recovered.
If your pneumonia is so severe that you are treated in the hospital, you may be given intravenous fluids and antibiotics, as well as oxygen therapy, and possibly other breathing treatments.
Risk factors
Pneumonia can affect anyone. But the two age groups at highest risk are:
- First, children who are 2 years old or younger
- And, secondly people who are age 65 or older
Other risk factors include:
- Being hospitalized. You’re at greater risk of pneumonia if you’re in a hospital intensive care unit, especially if you’re on a machine that helps you breathe (a ventilator).
- Chronic disease. You’re more likely to get pneumonia if you have asthma, chronic obstructive pulmonary disease (COPD) or heart disease.
- Smoking. Smoking damages your body’s natural defenses against the bacteria and viruses that cause pneumonia.
- Weakened or suppressed immune system. People who have HIV/AIDS, who’ve had an organ transplant, or who receive chemotherapy or long-term steroids are at risk.
Possible Complication
People who may be more likely to have complications from pneumonia include:
- Older adults or very young children.
- People whose immune system does not work well.
- People with other, serious medical problems such as diabetes or cirrhosis of the liver.
- Respiratory failure, which requires a breathing machine or ventilator.
- Sepsis, is a condition in which there is uncontrolled inflammation in the body, which may lead to widespread organ failure.
- Acute respiratory distress syndrome (ARDS), a severe form of respiratory failure.
- Lung abscesses, which are infrequent, but serious complications of pneumonia. They occur when pockets of pus form inside or around the lung. These may sometimes need to be drained with surgery.
Prevention
To help prevent pneumonia:
- First, is getting vaccinated. Vaccines are available to prevent some types of pneumonia and the flu.
- Second, Make sure children get vaccinated. Doctors recommend a different pneumonia vaccine for children younger than age 2 and for children ages 2 to 5 years who are at particular risk of pneumococcal disease. Children who attend a group child care center should also get the vaccine. Doctors also recommend flu shots for children older than 6 months.
- Third , Practice good hygiene. To protect yourself against respiratory infections that sometimes lead to pneumonia, wash your han ds regularly or use an alcohol-based hand sanitizer.
- Furthermore Don’t smoke. Smoking damages your lungs’ natural defenses against respiratory infections.
- Keep your immune system strong. Get enough sleep, exercise regularly and eat a healthy diet.
*[ COVID-19]: coronavirus disease 2019