Osteoporosis: Treatment, Causes, and Symptoms
Author: Rose Stella
Rose Stella
Category: Health
Tags: health, bone, women's health, risk, osteoporosis

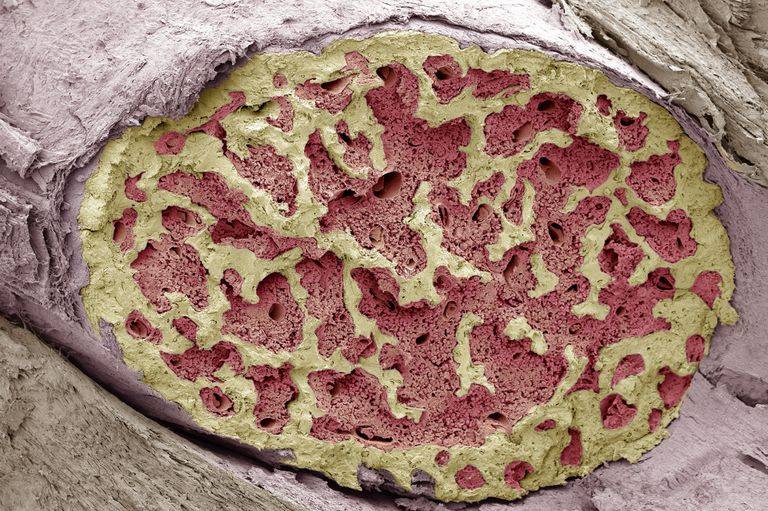
What is Osteoporosis?
Osteoporosis is one of the most prevalent bone diseases today. This condition is characterized by a decrease in the density of bone, decreasing its strength and resulting in fragile bones. In addition, the outside of the grows weaker and thinner, making it easy to break.
This is a bone disease that rarely shows symptoms. Its diagnosis often happens when there is a fracture or broken bones. In postmenopausal women and older men, osteoporosis is the leading cause of fractures. Fractures can occur in any bone, although the hip, vertebrae in the spine, and wrist are the most common.
What are the Symptoms of Osteoporosis?

The symptoms of this disease rarely show. It usually goes unnoticed until a bone breaks or one or more vertebrae collapses (fracture). Severe back discomfort, loss of height, or spine abnormalities such as a stooped or hunched posture are all symptoms.
Furthermore, some earlier symptoms also include receding gums, weakened grip strength and weak and brittle nails.
Osteoporosis-affected bones can become so weak that they shatter spontaneously or as a result of:
- Minor falls from positions that would unlikely to break a healthy bone.
- Bending, lifting, and even coughing are all common strains.
Causes of Osteoporosis
Osteoporosis happens when a large amount of bone mass is lost and when there is a structural change in the bone tissue. Some risk factors increase the chances of having the disease.
People who have osteoporosis have several risk factors while others don't. There are risk factors that are changeable and preventable. Learning about these risk factors is beneficial to prevent the disease or lessen its severity.
The following factors may raise your risk of having osteoporosis:
Sex
The chances of having osteoporosis are higher among women than men. Women have smaller bones and a lower peak bone mass than men. Men, on the other hand, are still at risk, particularly after the age of 70.
Age
New bone formation slows down with age. In addition, bones might deteriorate over time, increasing the risk of osteoporosis.
Body size.
Thin-boned women have a higher risk of having osteoporosis than larger-boned women because they have fewer bones to lose.
Race
White and Asian women are the most vulnerable when it comes to osteoporosis. Women of African and Mexican descent are at a lesser risk. African-American and Mexican-American males are at a higher risk than white men.
Family History.
Researchers have shown that if one of your parents has had osteoporosis or hip fracture, your risk of developing osteoporosis and fractures is high.
Changes in hormones.
Low levels of certain hormones can make an individual more susceptible to osteoporosis. For instance, low estrogen levels in women following menopause and low testosterone level in men.
Low estrogen levels result from premenopausal women’s abnormal lack of monthly periods, which can be caused by hormone abnormalities or excessive physical activity. On the other hand, the progressive decline of testosterone with age doesn’t equate to a substantial cause of bone loss.
Diet

A low-calcium, low-vitamin D diet can increase an individual risk of osteoporosis and fractures from childhood through old life. For instance, excessive calorie restriction.
Medications
Long-term use of certain medicines may make an individual more likely to develop bone loss and osteoporosis. For instance, medicine such as:
- Glucocorticoids and adrenocorticotropic hormones, which treat various conditions, such as asthma and rheumatoid arthritis.
- Antiepileptic medicines, which treat seizures and other neurological disorders.
- Cancer medications, which use hormones to treat breast and prostate cancer.
- Proton pump inhibitors, which lower stomach acid.
- Selective serotonin reuptake inhibitors, which treat depression and anxiety.
- Thiazolidinediones, which treat type II diabetes.
Unhealthy Lifestyle. Some lifestyle increases the risk of having osteoporosis. Excessive alcohol drinking and smoking make an individual more susceptible to the disease.
Diagnosis of Osteoporosis
To diagnose osteoporosis, the doctors will need to review the medical history and do a physical exam. Running blood tests and urine tests are necessary to check the physical condition of an individual.
When the results suggest that the patient has a high chance of having this medical condition, the doctor will suggest a bone density test. This test is called bone densitometry, or dual-energy X-ray absorptiometry (DEXA). It employs X-rays to determine the density of your wrists, hips, and spine bones. These are the three regions where this disease is most likely to occur. This non-invasive exam might take anywhere from 10 to 30 minutes to complete.
Treatment for Osteoporosis
Osteoporosis treatment aims to decrease or stop bone loss while also preventing fractures. Your doctor may advise you to do the following:
Proper nutrition is essential.
Having proper nutrition is needed to lessen the risk of having osteoporosis in the later years of life. This means living and eating healthy. For instance, adding fruits and vegetables to the meal plan is a must. It is also beneficial, to eat the right amount of food that is proportionate to one's age, height, and weight. In addition, adding foods and liquids-rich in calcium, vitamin D and protein would help maximize bone health.
Changes in your way of life.
A healthy lifestyle, in addition to balanced food, is critical for bone health. Avoiding being exposed to secondhand smoke and quitting smoking is a must. In addition, decreasing alcohol intake is also necessary. Furthermore, regularly seeing your doctor for check-ups and inquiries about medical conditions is also advised.

Excercise
Exercise is an essential component of an osteoporosis treatment plan. Strength training and resistance training are the best physical activities for bone health, according to research. Exercise can strengthen bones during childhood and adulthood since bone is live tissue. Exercise, on the other hand, does not increase bone mass in older persons.
Regular exercise can benefit older persons by improving their coordination and balance while increasing muscle mass and strength. It also improves daily function and puts off the loss of independence as long as possible.
While exercise is useful for persons with osteoporosis, it should not put your bones under undue stress. High-impact exercise should be avoided for people who suffer from this disease.
Medications
There are available prescriptions for osteoporosis but like any other medicine, it also has its drawbacks. It is important to ask for a doctor's prescription for the best suitable medication for those people who have osteoporosis.