Athlete’s foot: Causes and Treatment
Author: Rose Stella
Rose Stella
Category: Health
The athlete’s foot is a fungus that starts between the toes and spreads to the rest of the foot. It is most common in persons who have sweaty feet from being constrained in tight-fitting shoes.
An itchy, scaly rash is one of the signs and symptoms of an athlete’s foot. The illness is contagious and can be passed on through contaminated flooring, towels, or clothing.
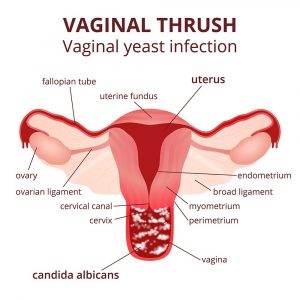
Other fungal infections, such as ringworm and jock itch, are closely related to the athlete’s foot. Antifungal drugs can be used to treat it, but the infection commonly returns.
What Causes Athlete's Foot?
Athletes’ foot is caused by a variety of factors.
When the tinea fungus spreads on the feet, it is known as the athlete’s foot. You can contract the fungus by coming into direct contact with an affected individual or touching fungus-infested surfaces. Warm, damp surroundings are ideal for the fungus to thrive. Showers, locker room floors, and swimming pools are all frequent places to find it.
An athlete’s foot can affect anyone regardless of any demographics. Anyone can have Athlete's foot.
An athlete’s foot can affect anyone, but specific behaviors make it more likely. Athlete’s foot can be caused by several factors, such as sharing socks, shoes, or towels with an infected individual wearing tight, closed-toe shoes in public locations, including locker rooms, showers, and swimming pools. Having sweaty feet having a minor skin or nail injury on your foot keeps your feet wet for long periods.
Different Types of Athlete's Foot
If your feet are always burning or itchy, and you notice a rash on your skin, you may have an athlete’s foot. But did you realize that there are several different types?
This infection is caused by a fungus. Walking barefoot in places where bacteria congregate, such as public pools or gym locker rooms, is one of the most common ways to catch it. If you share socks, bath towels, or bed sheets with someone who already has it, you can get them.
The specific symptoms of an athlete’s foot vary depending on the type of infection you have. Red, blistery rashes are caused by some types. Your skin may appear thick and scaly to others. So, which one do you think you have?
Toe Web Infection

Toe web infection is an interdigital infection. That just means it’s between the toes or fingers.
It commonly begins between your fourth and fifth toes on the skin or the pinkies. Bacteria can sometimes take hold and exacerbate the fungal infection.
Symptoms: A burning sensation between your toes is possible. The rash may be red, peeling, or scaly, and it may smell or produce a discharge. In severe situations, your skin may turn a bluish-green tint.
Moccasin Infection

A moccasin infection occurs when the fungus covers the sole of your foot. The rash may also travel up the side of your foot and along your heel.
Symptoms: Your feet may feel painful, dry, or somewhat itching at first. The skin thickens, splits, or peels after a while.
Your toenails may become thick and crumbly if the infection spreads to your nails. The nails may even come out at times.
You won’t be able to apply a topical treatment. It’s sometimes preferable to use a combination of drugs, including one specifically for your nails.
Vesicular Infection

Blisters are called vesicles in medical terms, and that’s exactly what this form of infection looks like. If the blisters pop, you may get a bacterial infection that necessitates antibiotic treatment.
Vesicular infections can affect any part of your foot. The little, red blisters, on the other hand, generally appear on your soles or between your toes. Itchy or severe rashes are possible. In the heat, it might be even worse.
Ulcerative Infection

It’s uncommon, but feet can sometimes develop open sores or ulcers. Those ulcers are also susceptible to bacterial infection. Antibiotics will be required to treat this.
Symptoms: Your skin becomes exceedingly irritated and pigmented, in addition to ulcers that may exude drainage. This infection is generally excruciatingly painful.
How to diagnose, treat, and prevent athlete’s foot.
You can continue to use some drugstore remedies to prevent an athlete’s foot from reappearing. It’s also critical to maintaining a clean and dry environment for your feet. You are not required to miss work or school.
Things to do to cure Athlete’s foot
- After washing your feet, dab them dry rather than rubbing them dry, especially between your toes.
- Use a separate towel for your feet that you may wash on a regular basis.
- When you’re at home, remove your shoes.
- Clean socks should be worn every day – cotton socks are ideal.
Things to avoid to cure Athlete’s foot
- Scratching the damaged skin might spread the infection to other regions of your body.
- Wear flip-flops in locations like changing rooms and showers instead of walking around barefoot.
- Do not use other people’s towels, socks, or shoes.
- Wearing the same pair of shoes for more than two days in a row is not recommended.
- Wearing shoes that make your feet sweaty and heated is not a good idea.
What is the treatment for the athlete’s foot?
Over-the-counter (OTC) topical antifungal medicines are treatments for the athlete’s foot. If over-the-counter drugs don’t work, your doctor may prescribe prescription-strength antifungal treatments. Your doctor may also suggest home remedies to help you get rid of the infection.
OTC (over-the-counter) drugs
There are a variety of over-the-counter antifungal medicines available, including:
- miconazole (Desenex)
- terbinafine (Lamisil AT)
- clotrimazole (Lotrimin AF)
- butenafine (Lotrimin Ultra)
- tolnaftate (Tinactin)
Medications on prescription
For athlete’s foot, your doctor may prescribe the following prescription medications:
- Oral antifungal drugs such as itraconazole (Sporanox), fluconazole (Diflucan), or prescription-strength terbinafine (Lamisil)
- Topical steroid treatments to relieve unpleasant inflammation
- Oral antibiotics if bacterial infections arise due to raw skin and blisters
Care at home
To help blisters dry out, your doctor may recommend soaking your feet in saltwater or diluted vinegar.
If your symptoms persist or worsen, you’ll need to see your doctor for an antibiotic prescription.