Myelodysplastic Syndromes
Author: Alvin
Alvin
Category: Health
Tags: health, men's health, blood, mds, women's health, child's health, cells
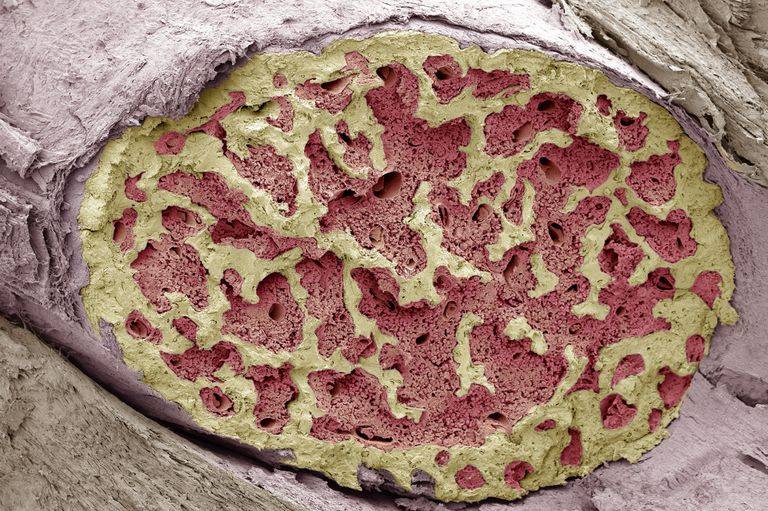
Myelodysplastic syndromes are a collection of diseases that are brought on by abnormally produced or dysfunctional blood cells. These conditions can be either inherited or acquired. Myelodysplastic syndromes are the result of abnormalities in the spongy material. That is found inside your bones and is responsible for the production of blood cells (bone marrow).
The goal of treatment for myelodysplastic syndromes is often to delay the progression of the disease. Also, improve symptoms, and protect against consequences. Blood transfusions and the use of drugs that stimulate the creation of blood cells are both common treatments. A bone marrow transplant, also known as a stem cell transplant. It may be advised to replace your own bone marrow with healthy bone marrow from a donor in certain circumstances. This procedure is also known as a stem cell transplant.
All of these conditions are distinguished by the presence of one or more peripheral blood cytopenias. The bone marrow is typically hypercellular, although on occasion. A hypocellular marrow that resembles aplastic anemia may observed. Cells in the bone marrow have abnormal morphology and do not mature properly. (This condition known as dysmyelopoiesis). Which leads to inefficient generation of blood cells.
Normal Bone Marrow
 The different types of myelodysplastic syndromes are
diagnosed based on certain changes in the blood cells and bone marrow.
The different types of myelodysplastic syndromes are
diagnosed based on certain changes in the blood cells and bone marrow.
Bones include bone marrow. It contains blood-forming, fat, and sustaining cells. Few blood-forming cells are stem cells. New blood cells need stem cells.
Blood cells are red, white, and platelets.
Red blood cells take oxygen from the lungs and deliver it to the body. These cells return CO2 to the lungs. Anemia is low red blood cells. It can cause fatigue, weakness, and pallor. Anemia can cause breathlessness.
Leukocytes (white blood cells) help fight infection. White blood cells are diverse.
Granulocytes have microscopic granules. Myeloblasts become granulocytes in bone marrow. Neutrophil is most common granulocyte. Neutropenia decreased blood neutrophils. Infections can result.
Monocytes help fight pathogens. Bone marrow monoblasts become monocytes.
Lymphocytes generate antibodies to fight pathogens. They kill microorganisms. MDS seldom affects lymphocytes.
Platelets aren’t blood cells; they’re cell fragments. Megakaryocytes are their bone marrow origin. Platelets are fragments of this cell. Platelets clot blood. They plug cut or bruised blood vessels. Thrombocytopenia causes abnormal bleeding and bruising.
Types of Myelodysplastic Syndromes
Myelodysplastic syndromes, often known as MDS. They are categorized using the classification system developed by the World Health Organization (WHO). Which was most recently revised in the year 2016. It categorizes MDS into different categories based mostly on the appearance of the cells in the bone marrow. When viewed through a microscope, in addition to taking into account the following factors:
How many of the early forms of cell types seen in the bone marrow. (Such as red blood cells, white blood cells, or platelets) show signs of dysplasia?
In how many different types of low blood cell counts (cytopenias) an individual suffers from.
How much of the first red blood cells are made up of ring sideroblasts? (Cells that contain rings of iron deposits around the nucleus).
The quantity of blasts, which are very early kinds of blood cells. That can be found in the blood or bone marrow.
Alterations in certain chromosomes in the cells of the bone marrow.
MDS with multilineage dysplasia (MDS-MLD)
At least 10 percent of the early cells of two or three different cell types. (Red blood cells, white blood cells, and/or megakaryocytes [the cells that create platelets.]) nI the bone marrow show signs of dysplasia. These cell types include red blood cells, white blood cells, and megakaryocytes.
At least one type of blood cell is present in inadequate quantities in the individual.
In the bone marrow, the amount of very early cells known as blasts is considered to be normal. (Less than 5 percent), whereas in the blood, blasts are extremely uncommon or nonexistent.
This particular variety of MDS is by far the most typical. In the past, people used to talk about this condition under the name. “Refractory cytopenia with multilineage dysplasia” (RCMD).
MDS with single lineage dysplasia (MDS-SLD)
At least 10% of early red, white, or platelet-making megakaryocytes in the bone marrow are dysplastic.
The person has low levels of one or two blood cell types but normal numbers of another (s).
In the bone marrow, very early cells called blasts are infrequent (or nonexistent).
Rare MDS. AML seldom advances (AML). Even without treatment, patients with this kind of MDS frequently live long lives.
RCUD was the prior categorization for this condition. Depending on the cell type, it comprises refractory anemia, neutropenia, and thrombocytopenia.
Type with ring sideroblasts (MDS-RS)
Early red blood cells in this MDS are ring sideroblasts. 15% of early red blood cells must be ring sideroblasts for this diagnosisO (or at least 5 percent if the cells also have a mutation in the SF3B1 gene).
This condition is classified into 2 kinds based on how many bone marrow cell types affected:
MDS-RS-SLD: dysplasia in one cell type.
MDS-RS-MLD: dysplasia in many cell types.
Rare MDS. It rarely becomes AML and has a better prognosis than other MDS forms. Refractory anemia with ring sideroblasts (RARS).
Clinical classification
 Age and past treatment with chemotherapy or radiation
therapy affect the risk of a myelodysplastic syndrome.
Age and past treatment with chemotherapy or radiation
therapy affect the risk of a myelodysplastic syndrome.
MDS can categorized not only according to the criteria established by the WHO. But also according to the underlying cause. This kind of categorization called a clinical classification.
It referred to as primary MDS when there is no identifiable etiology. (The frequency of this kind is higher.)
The condition referred to as secondary MDS when it known what caused the disease.
Secondary myelodysplastic syndrome frequently associated with prior cancer therapy. Or it might develop in people who have already diagnosed with another bone marrow condition. In the section under “Risk Factors for Myelodysplastic Syndrome,” this topic explored in further depth.
It is essential to determine if a patient has primary or secondary MDS. Since the secondary variant of the disease is significantly less likely to respond to treatment.
Causes
The majority of instances of myelodysplastic syndrome (MDS) have unidentified causes. However, there are certain cases that can linked to known risk factors.
Researchers have made significant headway in their quest to understand. How particular alterations in the DNA of bone marrow cells may contribute to the development of MDS. DNA is the molecule that composes our genes. Which are responsible for determining how each of our cells works. Because our DNA comes from our parents, we often take after the appearance of our parents. However, DNA is responsible for far more than just our appearance.
Certain genes determine the rate at which our cells mature, divide to create new cells, and pass away:
Oncogenes are a category of genes that refer to genes that help cells grow, divide, and continue to exist.
Genes that contribute to the regulation of cell division or that prompt the death of cells. At the appropriate moment referred to as tumor suppressor genes.
Gene mutations, also known as gene defects, are a potential cause of cancer.
These mutations can either activate oncogenes or silence tumor suppressor genes.
Before a person can acquire myelodysplastic syndrome (MDS). Abnormalities in many genes inside the cells of the bone marrow typically required. DNMT3A mutations, TET2 mutations, ASXL1 mutations, TP53 mutations, RUNX1 mutations, SRSF2 mutations. And SF3B1 mutations are some of the most common types of MDS cell mutations. It is possible for a person to inherit one or more of these gene modifications from a parent. But it is much more common for these changes to take place during a person’s lifetime.
Prevention
There is no failsafe method available for avoiding myelodysplastic syndromes (MDS). However, there are things that you may take to potentially lessen the severity of the consequences.
Quitting smoking is one way to reduce one’s risk of myelodysplastic syndrome (MDS). Which associated with greater risk of smoking. Persons who don’t smoke naturally have a lower risk of developing a wide variety of other cancers. As well as heart disease, stroke, and a variety of other ailments, in comparison to people who do smoke.
It is possible that your risk of acquiring MDS will reduced if you steer clear of industrial chemicals. That known to cause cancer, such as benzene.
Radiation therapy and certain chemotherapy medicines have linked to an increased incidence of myelodysplastic syndrome (MDS). Researchers are looking on ways to reduce the likelihood of patients. Developing MDS as a result of receiving these medicines. When treating some types of cancer, medical professionals may make an effort to avoid using chemotherapy medications. That are more likely to cause myelodysplastic syndrome (MDS). However, it’s possible that certain individuals require these particular medications. In many cases, it is necessary to weigh the clear advantages of treating life- threatening malignancies. With chemotherapy and radiation therapy against the remote possibility of getting MDS a few years down the road.
Supportive Therapy
 Tests that examine the blood and bone marrow are used to
diagnose myelodysplastic syndromes.
Tests that examine the blood and bone marrow are used to
diagnose myelodysplastic syndromes.
In contrast to medications that directly treat myelodysplastic syndromes (MDS). Supportive therapies are treatments that help treat. Or prevent the symptoms of MDS or complications that may arise as a result of having MDS. MDS patients have the option of using supportive therapy alone or in conjunction. With other forms of treatment. No matter what stage the illness is at or what the ultimate goal of treatment might be. The primary objective of this kind of treatment is to enhance the level of comfort. And quality of life of a person who has diagnosed with cancer. You might also hear phrases like “symptom management” or “comfort care” or “palliative care” used interchangeably with “supportive care.”
For many patients who have myelodysplastic syndrome (MDS). For instance, one of the primary aims of treatment is to avoid the complications. That brought on by having low blood cell counts.