Bronchiectasis: What You Need To Know
Author: Shiela Lupiba
Shiela Lupiba
Category: Fitness
Tags: health, mucus, bronchiectasis, lungs, fitness

What is Bronchiectasis?
Bronchiectasis (pronounce as brong-kee-ek-tuh-sis) is a lung disease that causes mucus to be cough up. The bronchi are the airways in the lungs that allow air to enter. The interior surfaces of the bronchi thicken over time in bronchiectasis due to inflammation, leaving scars. Mucus collects in these tubes because the walls aren’t strong enough to keep the mucus from moving out of the lungs. Furthermore, the cilia (thin strands that resemble hair and aid in the movement of mucus) are destroy. Infections are more likely to occur as a result of this, and breathing becomes difficult. Exacerbations happen when breathing or coughing becomes more difficult.
CAUSES
Cystic fibrosis (CF), a hereditary disorder that causes long-term lung infections and a diminished ability to breathe, maybe the cause of bronchiectasis. CF deteriorates with time.
The cause of non-CF bronchiectasis is not usually familiar. Idiopathic bronchiectasis is the medical term for this condition. Other causes, on the other hand, include:
- Infections that have caused lung damage in the past
- Primary ciliary dyskinesia and alpha-1 antitrypsin deficiency are both genetic disorders.
- Illnesses of the immune system that make it difficult to combat infections
- Fluids, gastric acid, or meals are puff (breath in) into the lungs.
- An allergy to a specific type of fungus is know as allergic bronchopulmonary aspergillosis.
SYMPTOMS
Some of the most common symptoms are:
- Coughing that results in a lot of mucus
- Coughing up mucus that has blood in it (known as hemoptysis)
- Chest pain or tightness because it is harder to breathe
- Wheezing or making whistling noises when breathing
- Clubbing of nails
- Loss of weight
- Flare-ups that usually include:
- Fatigue
- Increased shortness of breath
- Night sweats
- Fever
If your doctor listens to your lungs with a stethoscope, he or she may hear abnormal lung sounds.
Over time, you may have more serious symptoms. You may cough up blood or bloody mucus and feel very tired. Children may lose weight or not grow at a normal rate.
RISK FACTORS
Bronchitis is a lung disease that affects people who have disorders that damage their lungs or make them more susceptible to infections. These are some of the conditions:
- Cystic fibrosis is a disease that affects the lungs. In the United States, this disease is responsible for over half of all occurrences of bronchiectasis.
- Immunodeficiency disorders, such as CVI and, less commonly, HIV and AIDS.
- Aspergillosis of the bronchopulmonary system caused by an allergic reaction. This is an allergic reaction to the aspergillus fungus. Swelling of the airways occurs as a result of the reaction.
- Primary ciliary dyskinesia is an example of a disorder that affects cilia function. Your airways are lined with cilia, which are little hair-like structures. They aid in the removal of mucus (a slimy substance) from your airways.
DIAGNOSIS
Bronchiectasis is an ailment that is under-diagnosed. If you have bronchiectasis, your doctor will first ask for a full family history and blood testing to see if you have an underlying ailment that could cause it. These blood tests can also reveal whether you have low numbers of infection-fighting blood cells, which your doctor can address.
Because it’s a lung condition, your doctor will want to check your lung function as well. They’ll begin by listening to your lungs for any obstructions or irregularities. Lung function tests might help you figure out how well your lungs are doing. A sputum culture can also tell your doctor if you have germs in your lungs.
A chest X-ray or CT scan is the most common approach to identify bronchiectasis once other reasons have been ruled out. Both tests produce thorough images of your lungs, heart, and airways, providing your doctor with a complete view of your condition.
Doctors may recommend a bronchoscopy in severe cases of bronchiectasis that isn’t responding to treatment. This flexible, narrow tube is placed into the airways to aid in the detection of obstructions and infection sources.
TREATMENTS
Treatment involves a combination of medicine, exercises you can learn, and devices to help clear your airways. Surgery for bronchiectasis is rarely required. Bronchiectasis is not curable, however, it can be manage. Your doctor may recommend medicine, the use of certain devices, or a mix of these and potentially other approaches.
Also, if bronchiectasis causes by an underlying condition, such as aspergillosis or an immune system disorder, the underlying ailment must give treatment first.
Medication may be used as a treatment option, such as:
- Antibiotics are antibiotics that are use to treat bacterial infections. Oral (pill) and gasp versions are among them (breath in using a nebulizer machine).
- Macrolides are anti-infectives and anti-inflammatory medications that work in tandem.
- Drugs that alter mucous and aid in the coughing up of mucus.
Treatment might also include:
- Airway clearance devices assist you cough up mucus and break it up.
- PEP devices (positive expiratory pressure) that you can hold in your hands
- Wearable percussion instruments, such as vests
- Mucus can be moved out of the body with physical therapy techniques like chest clapping.
- Treatment for bronchiectasis is also divided down by stage: there are certain things you must perform on a daily basis.
Early diagnosis and treatment of the underlying cause of bronchiectasis may help prevent further lung damage.
In addition, cystic fibrosis or immunodefiency or any diseases that associates with bronchiectasis should be treated.
LIST-TO-DO
Patients should work with their doctors to develop healthy practices that will help them avoid flare-ups. The following are some ideas:
- Stop smoking and stay away from secondhand smoke.
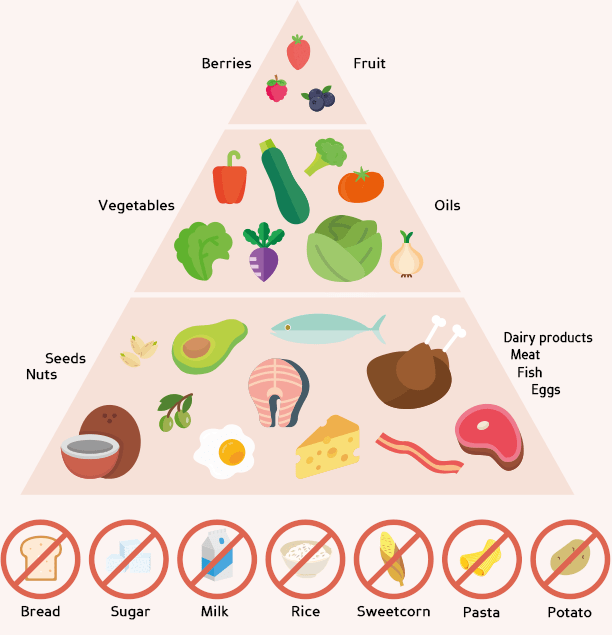
- Maintain a low-sodium, added-sugars, saturated-fat, and refined-grain diet.
- Keep yourself hydrated by drinking plenty of water to avoid mucus build-up.
- Take oral and inhalation drugs as directed and conduct mucus clearing treatments on a daily basis.
- Vaccinations are kept up to date.
- During flare-ups, use antibiotics for one to two weeks.
- Even if you live a healthy lifestyle, you may experience flare-ups from time to time. This is frequently caused by a new respiratory infection or bacterial overgrowth.
- ymptoms such as increased mucus (sputum) production that is bloody or a different color, fever, fatigue, weight loss and worsening shortness of breath may be a sign you're experiencing a flare-up. In these instances, you should contact your doctor immediately